Deck 5: Gastrointestinal System
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/102
Play
Full screen (f)
Deck 5: Gastrointestinal System
1
What increases the likelihood of reflux esophagitis?
A) Hiatal hernia.
B) Achalasia.
C) Portal hypertension.
D) Diverticula.
A) Hiatal hernia.
B) Achalasia.
C) Portal hypertension.
D) Diverticula.
Hiatal hernia.
2
Which of the following are digestive enzymes secreted by the pancreas?
(1)Trypsin.
(2)Chyme.
(3)Chymotrypsin.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3
(1)Trypsin.
(2)Chyme.
(3)Chymotrypsin.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3
1 and 3 only
3
A pear-shaped organ that lies on the undersurface of the liver is the
A) pancreas
B) spleen
C) gallbladder
D) duodenum
A) pancreas
B) spleen
C) gallbladder
D) duodenum
gallbladder
4
What is mastication?
A) Chewing.
B) Swallowing.
C) Solid waste excretion.
D) Rhythmic contractions that move digestive contents through the GI tract.
A) Chewing.
B) Swallowing.
C) Solid waste excretion.
D) Rhythmic contractions that move digestive contents through the GI tract.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
5
Failure of a satisfactory esophageal lumen to develop separate from the trachea is termed
A) tracheoesophageal fistula
B) achalasia
C) Barrett's esophagus
D) hiatal hernia
A) tracheoesophageal fistula
B) achalasia
C) Barrett's esophagus
D) hiatal hernia

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
6
What is the function of the gallbladder?
A) Produce bile.
B) Store and concentrate bile.
C) Produce trypsin.
D) Break down glycogen.
A) Produce bile.
B) Store and concentrate bile.
C) Produce trypsin.
D) Break down glycogen.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
7
What is the most common cause of acute esophagitis?
A) TE fistula.
B) Gastroesophageal reflux.
C) Infection.
D) Malignancy.
A) TE fistula.
B) Gastroesophageal reflux.
C) Infection.
D) Malignancy.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
8
Which of the following is a serious complication of TE fistula?
A) Hiatal hernia.
B) Gastroesophageal reflux disease (GERD).
C) Esophagitis.
D) Aspiration pneumonia.
A) Hiatal hernia.
B) Gastroesophageal reflux disease (GERD).
C) Esophagitis.
D) Aspiration pneumonia.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
9
An increase in glucose in the blood stimulates the beta cells in the _____ to secrete _____.
A) pancreas; insulin
B) pancreas; glucagon
C) liver; glycogen
D) liver; insulin
A) pancreas; insulin
B) pancreas; glucagon
C) liver; glycogen
D) liver; insulin

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
10
Deglutition is defined as
A) rhythmic contractions that move digestive contents through the GI tract
B) chewing
C) liquid waste excretion
D) swallowing
A) rhythmic contractions that move digestive contents through the GI tract
B) chewing
C) liquid waste excretion
D) swallowing

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
11
What condition is associated with severe reflux esophagitis?
A) Varices.
B) Barrett's esophagus.
C) Traction diverticula.
D) TE fistula.
A) Varices.
B) Barrett's esophagus.
C) Traction diverticula.
D) TE fistula.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
12
Which of the following is an emulsifier that aids in the breakdown of fats during digestion?
A) Bile.
B) Trypsin.
C) Pepsin.
D) Chyme.
A) Bile.
B) Trypsin.
C) Pepsin.
D) Chyme.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
13
Which organisms are most often responsible for infectious esophagitis?
A) Streptococcal bacteria and herpesvirus.
B) Helicobacter pylori bacteria and Candida fungus.
C) Herpesvirus and H. pylori bacteria.
D) Candida fungus and herpesvirus.
A) Streptococcal bacteria and herpesvirus.
B) Helicobacter pylori bacteria and Candida fungus.
C) Herpesvirus and H. pylori bacteria.
D) Candida fungus and herpesvirus.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
14
Smooth muscle contractions that move the contents of the digestive system along the GI tract are called
A) peristalsis
B) deglutition
C) mastication
D) emulsification
A) peristalsis
B) deglutition
C) mastication
D) emulsification

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
15
Where does the process of digestion begin?
A) Stomach.
B) Small intestine.
C) Mouth.
D) Esophagus.
A) Stomach.
B) Small intestine.
C) Mouth.
D) Esophagus.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
16
What is esophageal atresia?
A) An abnormal communication between the esophagus and the respiratory system.
B) Dilated, tortuous veins of the esophagus.
C) Functional obstruction causing proximal dilatation.
D) Congenital condition in which the esophagus ends in a blind pouch.
A) An abnormal communication between the esophagus and the respiratory system.
B) Dilated, tortuous veins of the esophagus.
C) Functional obstruction causing proximal dilatation.
D) Congenital condition in which the esophagus ends in a blind pouch.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
17
Acquired tracheoesophageal (TE)fistulas are commonly caused by
A) gastroesophageal reflux disease (GERD)
B) Barrett's esophagus
C) malignancy in the mediastinum
D) portal hypertension
A) gastroesophageal reflux disease (GERD)
B) Barrett's esophagus
C) malignancy in the mediastinum
D) portal hypertension

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
18
Where does the greatest amount of digestion occur?
A) Stomach.
B) Duodenum.
C) Jejunum.
D) Colon.
A) Stomach.
B) Duodenum.
C) Jejunum.
D) Colon.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
19
What is the largest gland in the body?
A) Pancreas.
B) Thyroid.
C) Adrenals.
D) Liver.
A) Pancreas.
B) Thyroid.
C) Adrenals.
D) Liver.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
20
The most common type of congenital TE fistula is
A) type I
B) type II
C) type III
D) type IV
A) type I
B) type II
C) type III
D) type IV

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
21
Which imaging modality is used to stage esophageal carcinoma?
A) Double-contrast barium swallow.
B) CT.
C) Ultrasound.
D) Nuclear medicine.
A) Double-contrast barium swallow.
B) CT.
C) Ultrasound.
D) Nuclear medicine.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
22
What is the most common abnormality found on upper GI exams?
A) Hiatal hernia.
B) Esophageal varices.
C) Esophageal diverticula.
D) Gastric ulcer.
A) Hiatal hernia.
B) Esophageal varices.
C) Esophageal diverticula.
D) Gastric ulcer.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
23
Which type of diverticulum arises in the distal 10 cm of the esophagus?
A) Zenker's.
B) Pulsion.
C) Traction.
D) Epiphrenic.
A) Zenker's.
B) Pulsion.
C) Traction.
D) Epiphrenic.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
24
Which of the following is strongly correlated with esophageal carcinoma?
(1)Excessive alcohol intake.
(2)Smoking.
(3)Portal hypertension.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3
(1)Excessive alcohol intake.
(2)Smoking.
(3)Portal hypertension.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
25
Perforation of the esophagus may be a complication of all of the following except
A) neoplasm
B) instrumentation
C) peptic ulcer
D) hiatal hernia
A) neoplasm
B) instrumentation
C) peptic ulcer
D) hiatal hernia

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
26
Which imaging procedure is used to detect esophageal carcinoma?
A) CT.
B) NM.
C) US.
D) Double-contrast barium swallow.
A) CT.
B) NM.
C) US.
D) Double-contrast barium swallow.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
27
Refer to the image.What esophageal pathologic condition is demonstrated? 
From Eisenberg RL: Gastrointestinal radiology: a pattern approach,Philadelphia,1990,Lippincott.
A) Varices.
B) Hiatal hernia.
C) Barrett's esophagus.
D) Esophageal diverticulum.
From Eisenberg RL: Gastrointestinal radiology: a pattern approach,Philadelphia,1990,Lippincott.
A) Varices.
B) Hiatal hernia.
C) Barrett's esophagus.
D) Esophageal diverticulum.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
28
Which of the following are complications of peptic ulcer disease?
(1)Hemorrhage.
(2)Obstruction.
(3)Perforation.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3
(1)Hemorrhage.
(2)Obstruction.
(3)Perforation.
A) 1 and 2 only
B) 1 and 3 only
C) 2 and 3 only
D) 1, 2, and 3

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
29
Which type of diverticulum arises from the posterior wall of the cervical esophagus?
A) Traction.
B) Pulsion.
C) Zenker's.
D) Epiphrenic.
A) Traction.
B) Pulsion.
C) Zenker's.
D) Epiphrenic.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
30
Which imaging procedure is used to demonstrate dilated veins in the walls of the esophagus?
A) Upper GI.
B) Barium enema.
C) MRI.
D) Double-contrast barium swallow.
A) Upper GI.
B) Barium enema.
C) MRI.
D) Double-contrast barium swallow.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
31
Where is the most common location of gastric ulcers?
A) Fundus.
B) Body.
C) Lesser curvature.
D) Greater curvature.
A) Fundus.
B) Body.
C) Lesser curvature.
D) Greater curvature.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
32
What is the most common manifestation of peptic ulcer disease?
A) Gastric ulcer in fundus.
B) Duodenal ulcer.
C) Gastric ulcer on lesser curvature.
D) Esophageal ulcer.
A) Gastric ulcer in fundus.
B) Duodenal ulcer.
C) Gastric ulcer on lesser curvature.
D) Esophageal ulcer.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
33
Where in the stomach do most gastric cancers occur?
A) Fundus.
B) Cardiac antrum.
C) Body.
D) Distal stomach.
A) Fundus.
B) Cardiac antrum.
C) Body.
D) Distal stomach.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
34
Which type of esophageal diverticulum contains all layers of the wall?
A) Traction.
B) Pulsion.
C) Zenker's.
D) Epiphrenic.
A) Traction.
B) Pulsion.
C) Zenker's.
D) Epiphrenic.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
35
What is the most common cause of dilated veins in the walls of the esophagus?
A) Abnormal function of the lower esophageal sphincter.
B) Reflux of abdominal contents into the esophagus.
C) Portal hypertension.
D) Weakness in the vessel wall.
A) Abnormal function of the lower esophageal sphincter.
B) Reflux of abdominal contents into the esophagus.
C) Portal hypertension.
D) Weakness in the vessel wall.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
36
Which imaging modality is used to stage gastric carcinoma?
A) Ultrasound.
B) Upper GI series.
C) CT.
D) MRI.
A) Ultrasound.
B) Upper GI series.
C) CT.
D) MRI.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
37
Difficulty swallowing is termed
A) deglutition
B) mastication
C) dysphagia
D) aphasia
A) deglutition
B) mastication
C) dysphagia
D) aphasia

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
38
What is the most common cause of acute gastrointestinal bleeding?
A) Peptic ulcer disease.
B) Esophageal varices.
C) Esophageal diverticula.
D) Gastric cancer.
A) Peptic ulcer disease.
B) Esophageal varices.
C) Esophageal diverticula.
D) Gastric cancer.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
39
Refer to the image.This esophageal pathologic condition is described as resembling beads on a rosary.What pathologic condition is evident in this image? 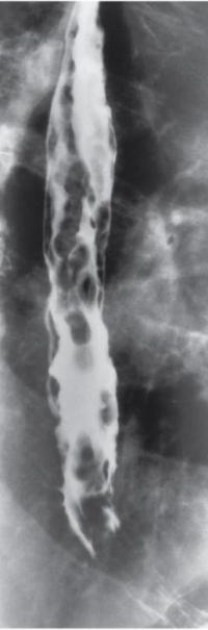
A) Varices.
B) Hiatal hernia.
C) Esophageal diverticula.
D) Gastric ulcer.
A) Varices.
B) Hiatal hernia.
C) Esophageal diverticula.
D) Gastric ulcer.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
40
Dilated veins in the walls of the esophagus are termed
A) diverticula
B) varices
C) dysphagia
D) achalasia
A) diverticula
B) varices
C) dysphagia
D) achalasia

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
41
Which of the following is one of the most typical forms of primary colon cancer?
A) Polypoid.
B) Fungating.
C) Ulcerative.
D) Annular.
A) Polypoid.
B) Fungating.
C) Ulcerative.
D) Annular.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
42
Which of the following is a major cause of bowel obstruction in children?
A) Volvulus.
B) Intussusception.
C) Abdominal surgery.
D) Intraluminal neoplasm.
A) Volvulus.
B) Intussusception.
C) Abdominal surgery.
D) Intraluminal neoplasm.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
43
What is one of the most common causes of obstruction in the large bowel?
A) Intussusception.
B) Primary colon cancer.
C) Volvulus.
D) Appendicitis.
A) Intussusception.
B) Primary colon cancer.
C) Volvulus.
D) Appendicitis.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
44
Which of the following is an ominous complication of ulcerative colitis?
A) Hemorrhage.
B) Toxic megacolon.
C) Obstruction.
D) Perforation.
A) Hemorrhage.
B) Toxic megacolon.
C) Obstruction.
D) Perforation.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
45
Refer to the image below.This typical saw-tooth configuration demonstrated on a barium enema exam is evidence of 
A) ulcerative colitis
B) diverticulosis
C) appendicitis
D) intussusception

A) ulcerative colitis
B) diverticulosis
C) appendicitis
D) intussusception

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
46
A common disorder of intestinal motor activity in which fluid and gas do not progress normally through an unobstructed bowel is called
A) regional enteritis
B) adynamic ileus
C) intussusception
D) ischemic colitis
A) regional enteritis
B) adynamic ileus
C) intussusception
D) ischemic colitis

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
47
Varicose veins of the lower end of the rectum that cause symptoms of pain,itching,and bleeding are
A) volvulus
B) intussusception
C) hemorrhoids
D) Crohn's disease
A) volvulus
B) intussusception
C) hemorrhoids
D) Crohn's disease

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
48
A condition of acquired herniations of mucosa and submucosa through muscular layers at points of weaknesses of the bowel wall is known as
A) diverticulosis
B) ulcerative colitis
C) Crohn's colitis
D) volvulus
A) diverticulosis
B) ulcerative colitis
C) Crohn's colitis
D) volvulus

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
49
A twisting of the bowel on itself that may lead to obstruction is termed
A) intussusception
B) colitis
C) appendicitis
D) volvulus
A) intussusception
B) colitis
C) appendicitis
D) volvulus

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
50
What is the current imaging modality of choice for the gallbladder?
A) Nuclear medicine.
B) Ultrasound.
C) Radiography.
D) CT.
A) Nuclear medicine.
B) Ultrasound.
C) Radiography.
D) CT.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
51
Which of the following technical adjustments is required when imaging a patient with known obstruction of the large bowel?
A) Increase in kVp.
B) Decrease in kVp.
C) Increase in kVp and double mAs.
D) Decrease in kVp and half mAs.
A) Increase in kVp.
B) Decrease in kVp.
C) Increase in kVp and double mAs.
D) Decrease in kVp and half mAs.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
52
Progressive shortening and rigidity of the colon and absent haustral patterns are radiographic evidence of
A) appendicitis
B) diverticulosis
C) diverticulitis
D) chronic ulcerative colitis
A) appendicitis
B) diverticulosis
C) diverticulitis
D) chronic ulcerative colitis

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
53
A chronic inflammatory disorder of unknown cause that often affects the terminal ileum is called
A) Crohn's disease
B) malabsorption syndrome
C) diverticulosis
D) gastritis
A) Crohn's disease
B) malabsorption syndrome
C) diverticulosis
D) gastritis

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
54
Which imaging modality is the gold standard for appendicitis?
A) Radiography (KUB).
B) Fluoroscopy (barium enema).
C) CT.
D) MRI.
A) Radiography (KUB).
B) Fluoroscopy (barium enema).
C) CT.
D) MRI.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
55
Which type of gallstone is most prevalent in the United States?
A) Cholesterol.
B) Pigment.
C) Mixed cholesterol and calcium carbonate.
D) None of these. Gallstones are rare in the United States.
A) Cholesterol.
B) Pigment.
C) Mixed cholesterol and calcium carbonate.
D) None of these. Gallstones are rare in the United States.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
56
Where in the colon do most primary cancers arise?
A) In preexisting polyps.
B) In diverticula.
C) In the perianal area.
D) In the ileocecal valve.
A) In preexisting polyps.
B) In diverticula.
C) In the perianal area.
D) In the ileocecal valve.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
57
What is intussusception?
A) A twisting of the bowel on itself.
B) A type of inflammatory bowel disease of unknown cause, with an associated psychogenic element.
C) Acquired herniation of the mucosa and submucosa of the intestinal wall.
D) The telescoping of one part of the intestinal tract into another.
A) A twisting of the bowel on itself.
B) A type of inflammatory bowel disease of unknown cause, with an associated psychogenic element.
C) Acquired herniation of the mucosa and submucosa of the intestinal wall.
D) The telescoping of one part of the intestinal tract into another.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
58
In which age group is appendicitis most common?
A) Infants and toddlers.
B) Children and adolescents.
C) Young adults.
D) Elderly adults.
A) Infants and toddlers.
B) Children and adolescents.
C) Young adults.
D) Elderly adults.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
59
The most common cause of a mechanical small bowel obstruction is
A) lack of peristalsis
B) intussusception
C) fibrous adhesions
D) volvulus
A) lack of peristalsis
B) intussusception
C) fibrous adhesions
D) volvulus

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
60
Which of the following is associated with prior cardiovascular disease?
A) Diverticulosis.
B) Ulcerative colitis.
C) Ischemic colitis.
D) Irritable bowel syndrome.
A) Diverticulosis.
B) Ulcerative colitis.
C) Ischemic colitis.
D) Irritable bowel syndrome.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
61
What is the most common cause of acute pancreatitis?
A) Blockage of pancreatic duct by impacted stone.
B) Diabetes.
C) Excessive alcohol consumption.
D) Cirrhosis.
A) Blockage of pancreatic duct by impacted stone.
B) Diabetes.
C) Excessive alcohol consumption.
D) Cirrhosis.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
62
Esophageal carcinoma is often detected early and carries a good prognosis.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
63
Gastric cancer is relatively rare in the United States.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
64
GERD is a common complication of hiatal hernia.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
65
Which of the following is appropriate when imaging a patient with known liver cirrhosis complicated by ascites?
A) Increase in kVp.
B) Decrease in kVp.
C) Increase in kVp and decrease in mAs by half.
D) Double mAs.
A) Increase in kVp.
B) Decrease in kVp.
C) Increase in kVp and decrease in mAs by half.
D) Double mAs.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
66
Hepatocellular carcinoma most commonly occurs in patients with
A) diffuse hepatocellular disease
B) chronic hepatitis
C) porcelain gallbladder
D) portal hypertension
A) diffuse hepatocellular disease
B) chronic hepatitis
C) porcelain gallbladder
D) portal hypertension

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
67
Esophageal varices are most commonly caused by a malfunction of the lower esophageal sphincter.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
68
What is the primary cause of acute cholecystitis?
A) Infection of the biliary system.
B) Cirrhosis of the liver.
C) Impacted gallstone in the cystic duct.
D) Peptic ulcer disease.
A) Infection of the biliary system.
B) Cirrhosis of the liver.
C) Impacted gallstone in the cystic duct.
D) Peptic ulcer disease.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
69
Pyloric stenosis usually results in
A) perforation of the pylorus
B) malabsorption syndrome
C) atrophy of the gastric mucosa
D) obstruction that prevents food from entering the duodenum
A) perforation of the pylorus
B) malabsorption syndrome
C) atrophy of the gastric mucosa
D) obstruction that prevents food from entering the duodenum

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
70
Esophageal atresia and TE fistula are often associated with other congenital malformations of the skeletal,cardiovascular,and gastrointestinal systems.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
71
Which imaging modality is the preferred method for the detection of pyloric stenosis?
A) Ultrasound.
B) MRI.
C) CT.
D) Radiography.
A) Ultrasound.
B) MRI.
C) CT.
D) Radiography.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
72
What is the modality of choice to image hepatocellular carcinoma?
A) Radiography.
B) CT.
C) MRI.
D) Nuclear medicine.
A) Radiography.
B) CT.
C) MRI.
D) Nuclear medicine.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
73
Which imaging modality is the most effective for detection of carcinoma of the pancreas?
A) Ultrasound.
B) Nuclear medicine.
C) MRI.
D) CT.
A) Ultrasound.
B) Nuclear medicine.
C) MRI.
D) CT.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
74
Refer to the image.This disorder is caused by a loss of bowel motility.What disorder is demonstrated in this abdominal radiograph? 
A) Mechanical obstruction.
B) Adynamic ileus.
C) Volvulus.
D) Intussusception.

A) Mechanical obstruction.
B) Adynamic ileus.
C) Volvulus.
D) Intussusception.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
75
Ascites is a common complication of liver cirrhosis.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
76
Which of the following is a sign of perforation of the GI tract?
A) Acute pancreatitis.
B) Pneumoperitoneum.
C) Pseudocysts.
D) Localized ileus.
A) Acute pancreatitis.
B) Pneumoperitoneum.
C) Pseudocysts.
D) Localized ileus.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
77
Peptic ulcer disease most commonly occurs in the duodenum.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
78
What condition results from chronic cholecystitis in which the gallbladder becomes fibrotic and calcified?
A) Cholecystectomy.
B) Pseudocyst.
C) Biliary carcinoma.
D) Porcelain gallbladder.
A) Cholecystectomy.
B) Pseudocyst.
C) Biliary carcinoma.
D) Porcelain gallbladder.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
79
Hiatal hernia is the most common disorder diagnosed on upper GI exams.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck
80
What is a common complication of cirrhosis?
A) Acute pancreatitis.
B) Portal hypertension.
C) Ascites.
D) Biliary obstruction.
A) Acute pancreatitis.
B) Portal hypertension.
C) Ascites.
D) Biliary obstruction.

Unlock Deck
Unlock for access to all 102 flashcards in this deck.
Unlock Deck
k this deck


