Deck 5: Coded Data
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/54
Play
Full screen (f)
Deck 5: Coded Data
1
Which organization is NOT one of the four Cooperating Parties for the ICD-10-CM?
A) American Medical Association (AMA)
B) Centers for Medicare and Medicaid Services (CMS)
C) National Center for Health Statistics (NCHS)
D) The Joint Commission (TJC)
A) American Medical Association (AMA)
B) Centers for Medicare and Medicaid Services (CMS)
C) National Center for Health Statistics (NCHS)
D) The Joint Commission (TJC)
American Medical Association (AMA)
2
Which is NOT a common use of coded data?
A) Reimbursement
B) Compliance
C) Scheduling
D) Research
A) Reimbursement
B) Compliance
C) Scheduling
D) Research
Scheduling
3
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 required the:
A) reporting of diagnosis data to the National Center for Health Statistics (NCHS).
B) adoption and use of ICD-10-CM.
C) use of the EHR with point-of-care data capture.
D) use of certain codes in electronic transmissions.
A) reporting of diagnosis data to the National Center for Health Statistics (NCHS).
B) adoption and use of ICD-10-CM.
C) use of the EHR with point-of-care data capture.
D) use of certain codes in electronic transmissions.
use of certain codes in electronic transmissions.
4
Why is electronic data interchange (EDI) beneficial?
A) computers can exchange information without human intervention
B) information can only be "read" by the recipient
C) messages contain unique identifiers that cannot be duplicated
D) it works across reimbursement and clinical platforms
A) computers can exchange information without human intervention
B) information can only be "read" by the recipient
C) messages contain unique identifiers that cannot be duplicated
D) it works across reimbursement and clinical platforms

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
5
What is Accredited Standards Committee (ASC) X12 Version 5010?
A) The code set used in inpatient settings for diagnoses
B) the electronic data interchange (EDI) standard used for electronic versions of the Uniform Bill
C) the name of the latest standard for transactions and code sets
D) the form used to assign procedure codes in ambulatory care
A) The code set used in inpatient settings for diagnoses
B) the electronic data interchange (EDI) standard used for electronic versions of the Uniform Bill
C) the name of the latest standard for transactions and code sets
D) the form used to assign procedure codes in ambulatory care

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
6
Current Procedure Terminology (CPT) is a
A) code set
B) electronic data interchange (EDI)
C) computer language
D) reference manual
A) code set
B) electronic data interchange (EDI)
C) computer language
D) reference manual

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
7
Current code sets under the Health Insurance Portability and Accountability Act (HIPAA) include all of the following, EXCEPT:
A) SNOMED CT.
B) National Drug Codes.
C) HCPCS and CPT-4.
D) ICD-10-CM and ICD-CM-PCS.
A) SNOMED CT.
B) National Drug Codes.
C) HCPCS and CPT-4.
D) ICD-10-CM and ICD-CM-PCS.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
8
A health care organization numbers its site locations not by geographic area or function, but by the order in which the sites were opened. For example, the head office is 001, the primary care physician group practice is 002, the urgent care office on the east side of town is 003, the imaging center is 004, and the urgent care office on the west side of town is 005. What type of coding system is this?
A) map
B) nomenclature
C) classification
D) taxonomy
A) map
B) nomenclature
C) classification
D) taxonomy

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
9
A list of preferred terms and their meanings is a
A) clinical vocabulary
B) nomenclature
C) data dictionary
D) taxonomy
A) clinical vocabulary
B) nomenclature
C) data dictionary
D) taxonomy

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
10
Tracking codes to determine the volume of cases seen at the facility is a _____________ use of coded data.
A) outcomes measurement
B) research
C) reimbursement
D) resource utilization
A) outcomes measurement
B) research
C) reimbursement
D) resource utilization

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
11
The way a code set is organized is its
A) clinical vocabulary
B) nomenclature
C) data dictionary
D) taxonomy
A) clinical vocabulary
B) nomenclature
C) data dictionary
D) taxonomy

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
12
0D5N4ZZ Destruction of Sigmoid Colon, Perc Endo Approach, is an example of a code from which code set?
A) ICD-9-PCS
B) ICD-10-PCS
C) SNOMED CT
D) DSM-IV
A) ICD-9-PCS
B) ICD-10-PCS
C) SNOMED CT
D) DSM-IV

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
13
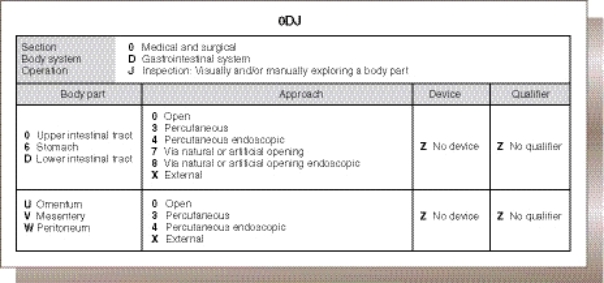
The second character of the code 0DJ86ZZ indicates which of the following?
A) Root Operation
B) Device
C) Body System
D) Approach
A) Root Operation
B) Device
C) Body System
D) Approach

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
14
The 5th character of the code 0DJ76ZZ indicates which of the following?
A) Location
B) Device
C) Body System
D) Approach
A) Location
B) Device
C) Body System
D) Approach

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
15
An example of a CPT-4 (Health Care Common Procedure Coding System [HCPCS] Level 1) code is:
A) C1715
B) 0DJD8ZZ
C) 4557003
D) 43251
A) C1715
B) 0DJD8ZZ
C) 4557003
D) 43251

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
16
The first three characters of an ICD-10-CM code represent the code:
A) etiology.
B) severity.
C) category.
D) anatomic site.
A) etiology.
B) severity.
C) category.
D) anatomic site.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
17
The NDC code for one 28-tablet bottle of the chronic hepatitis medication Harvoni, made by Gilead Sciences, is 61958-1801-1. The number "61958" is the
A) labeler code
B) product code
C) packaging code
D) batch code
A) labeler code
B) product code
C) packaging code
D) batch code

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
18
Which code set is alphanumeric?
A) ICD-10-PCS
B) NDC
C) CPT-4, Category 1
D) SNOMED CT
A) ICD-10-PCS
B) NDC
C) CPT-4, Category 1
D) SNOMED CT

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
19
Which organization does NOT develop, report, or maintain a classification and/or code set for health care purposes?
A) The Joint Commission.
B) the AMA.
C) the American Psychiatric Association (APA).
D) the International Health Terminology Standards Development Organization (IHTSDO).
A) The Joint Commission.
B) the AMA.
C) the American Psychiatric Association (APA).
D) the International Health Terminology Standards Development Organization (IHTSDO).

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
20
Which statement about SNOMED CT is false?
A) it can assign codes from free text
B) it makes systems interoperable across countries and languages
C) there is a one-to-one translation between SNOMED CT and ICD-10-CM
D) it has the potential to be useful during patient care, rather than after
A) it can assign codes from free text
B) it makes systems interoperable across countries and languages
C) there is a one-to-one translation between SNOMED CT and ICD-10-CM
D) it has the potential to be useful during patient care, rather than after

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
21
Which classification system is used to track neoplasms?
A) SNOMED CT
B) ICD-10-CM
C) ICD-O
D) CDT
A) SNOMED CT
B) ICD-10-CM
C) ICD-O
D) CDT

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
22
The _________ axis of an ICD-O-3 code indicates the site of a neoplasm in the body.
A) morphology
B) oncology
C) topography
D) pathology
A) morphology
B) oncology
C) topography
D) pathology

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
23
In an ICD-O-3 code, which part is the behavior code, indicating whether a tumor is malignant, benign, in situ, or uncertain?
A) the first four digits of the morphology axis
B) after the slash on the morphology axis
C) the letter character on the topographical axis
D) the numerical characters on the topographical axis
A) the first four digits of the morphology axis
B) after the slash on the morphology axis
C) the letter character on the topographical axis
D) the numerical characters on the topographical axis

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
24
Which is a requirement for a valid ICD-10-CM code?
A) has seven characters
B) begins with a letter character.
C) ends with a letter
D) has a dot
A) has seven characters
B) begins with a letter character.
C) ends with a letter
D) has a dot

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
25
A character value of X in the Qualifier position of certain ICD-10-PCS codes indicates a(n):
A) placeholder for the 7th character.
B) biopsy.
C) external approach.
D) device left in the body.
A) placeholder for the 7th character.
B) biopsy.
C) external approach.
D) device left in the body.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
26
In the third character of an ICD-10-PCS code, the main difference between the definitions of the Root Operations excision and resection is:
A) excision involves cutting out of or off, without replacement, all of a body part, while in a resection the body part is replaced.
B) excision involves cutting out of or off, with replacement, all of a body part; while in a resection all of a body part is cut off but no replaced.
C) excision involves cutting out of or off a portion of a body part; a resection involves cutting all of a body part out of or off.
D) excision involves cutting out of or off a portion of a body part, while a resection involves cutting out of or off all of a body part.
A) excision involves cutting out of or off, without replacement, all of a body part, while in a resection the body part is replaced.
B) excision involves cutting out of or off, with replacement, all of a body part; while in a resection all of a body part is cut off but no replaced.
C) excision involves cutting out of or off a portion of a body part; a resection involves cutting all of a body part out of or off.
D) excision involves cutting out of or off a portion of a body part, while a resection involves cutting out of or off all of a body part.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
27
Using the figure, which is the ICD-10-PCS code for an endoscopic colonoscopy? 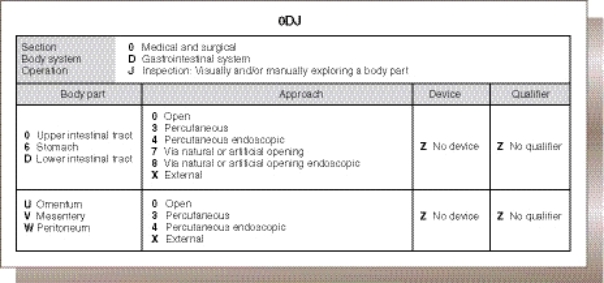
A) ODJD8ZZ
B) ODJD7ZZ
C) ODJ68ZZ
D) ODJ67ZZ
A) ODJD8ZZ
B) ODJD7ZZ
C) ODJ68ZZ
D) ODJ67ZZ

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
28
The auditor was reviewing the hospital bills and noticed that for several cases billed to a commercial payer the DRG assignment, based on the MS-DRG description of the DRG code, did not match the diagnosis/procedure codes. One possible reason for this is:
A) the coder made an error assigning the DRG.
B) the grouper isn't working properly.
C) that payer uses a different DRG than Medicare.
D) the MS-DRG description is incorrect.
A) the coder made an error assigning the DRG.
B) the grouper isn't working properly.
C) that payer uses a different DRG than Medicare.
D) the MS-DRG description is incorrect.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
29
What is the lowest level of medical complexity represented by CPT E/M codes?
A) straightforward
B) problem-focused
C) low complexity
D) detailed
A) straightforward
B) problem-focused
C) low complexity
D) detailed

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
30
Why might a coding manager automatically review and/or revise patients assigned to DRG 469 (MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W MCC) or DRG 470 (MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W/O MCC)?
A) The hospital might not be entitled to the reimbursement for these DRGs.
B) The federal government always reviews these DRGs for fraud and abuse.
C) There is something incorrect with the codes assigned and/or data when a patient is grouped into either of these DRGs.
D) These DRGs are on the OIG workplan this year.
A) The hospital might not be entitled to the reimbursement for these DRGs.
B) The federal government always reviews these DRGs for fraud and abuse.
C) There is something incorrect with the codes assigned and/or data when a patient is grouped into either of these DRGs.
D) These DRGs are on the OIG workplan this year.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
31
It is the coder's responsibility to assign codes completely and accurately so that a facility receives the reimbursement to which it is entitled. To meet this responsibility, a coder must:
A) follow all software prompts that will add a "cc" code. The software program is written so that the coder does not have to review the medical record.
B) use coding software to sequence the best principal diagnosis for the highest reimbursement.
C) code and sequence according to the documentation in the medical record, using the software to optimize the coding.
D) adjust the principle diagnosis as needed to achieve the right DRG for the patient's needs.
A) follow all software prompts that will add a "cc" code. The software program is written so that the coder does not have to review the medical record.
B) use coding software to sequence the best principal diagnosis for the highest reimbursement.
C) code and sequence according to the documentation in the medical record, using the software to optimize the coding.
D) adjust the principle diagnosis as needed to achieve the right DRG for the patient's needs.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
32
What software checks ICD-10 codes for age conflicts, such as a newborn jaundice code assigned to a middle-aged man?
A) the Medicare Code Editor (MCE)
B) the grouper
C) the encoder
D) the I-MAGIC algorithm
A) the Medicare Code Editor (MCE)
B) the grouper
C) the encoder
D) the I-MAGIC algorithm

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
33
Where does the grouper search for a comorbidity or complication (CC) or major comorbidity or complication (MCC)?
A) principal diagnosis codes
B) secondary diagnosis codes
C) E/M codes
D) SNOMED CT codes
A) principal diagnosis codes
B) secondary diagnosis codes
C) E/M codes
D) SNOMED CT codes

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
34
Why does the presence of a hospital-acquired condition (HAC) result in lower reimbursement?
A) it is relatively easy to treat
B) it is usually owing to a poor lifestyle choice by the patient
C) it is considered by Medicare to be preventable
D) it occurs mostly in areas with a lower cost of living
A) it is relatively easy to treat
B) it is usually owing to a poor lifestyle choice by the patient
C) it is considered by Medicare to be preventable
D) it occurs mostly in areas with a lower cost of living

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
35
What trend in the case mix might trigger a CMS audit?
A) an unusually high number of complex cases for a period of time
B) a large number of maternity and newborn cases
C) a decrease in MS-DRG complexity
D) fewer trauma patients
A) an unusually high number of complex cases for a period of time
B) a large number of maternity and newborn cases
C) a decrease in MS-DRG complexity
D) fewer trauma patients

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
36
A coder or group of coders is said to demonstrate ___________ when codes are consistently assigned for similar or identical cases.
A) reliability
B) validity
C) volume
D) compliance
A) reliability
B) validity
C) volume
D) compliance

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
37
____________ occurs when the coding results in the MS-DRG that most accurately represents the facility's utilization of resources, on the basis of the diagnoses and procedures, and is completely substantiated by documentation.
A) Maximization
B) Validity
C) Optimization
D) Compliance
A) Maximization
B) Validity
C) Optimization
D) Compliance

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
38
Which is the best way for HIM department managers to determine if charts are being coded at the proper volume?
A) monitoring volume data from coders in the facility over time
B) assuming the coder's role for a day and counting completed charts
C) comparing the volume data in a facility with the same number of beds
D) comparing the volume data in a facility with the same EHR system
A) monitoring volume data from coders in the facility over time
B) assuming the coder's role for a day and counting completed charts
C) comparing the volume data in a facility with the same number of beds
D) comparing the volume data in a facility with the same EHR system

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
39
How does computer-assisted coding (CAC) work?
A) the software scans specific free text and discrete data in the record and assigns codes
B) the coder looks up codes in a database
C) the provider selects codes from a drop-down menu
D) the software creates a diagnosis from vital signs, orders, and physician notes
A) the software scans specific free text and discrete data in the record and assigns codes
B) the coder looks up codes in a database
C) the provider selects codes from a drop-down menu
D) the software creates a diagnosis from vital signs, orders, and physician notes

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
40
Who audits the coding of Medicare patient records?
A) The Joint Commission
B) Quality Improvement Organizations (QIOs)
C) the state Board of Health
D) the state attorney general
A) The Joint Commission
B) Quality Improvement Organizations (QIOs)
C) the state Board of Health
D) the state attorney general

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
41
Why are coding audits performed by payers insufficient for determining coding accuracy?
A) the payer only checks records for the patients they have reimbursed
B) the payer only performs targeted reviews on "problem" DRGs
C) payers will only audit when there is a change in case mix
D) payers are ultimately more interested in volume rather than accuracy
A) the payer only checks records for the patients they have reimbursed
B) the payer only performs targeted reviews on "problem" DRGs
C) payers will only audit when there is a change in case mix
D) payers are ultimately more interested in volume rather than accuracy

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
42
An example of fraudulent and unethical coding is:
A) re-reviewing documentation after initial coding to search for a CC code or MCC code.
B) performing concurrent coding and questioning the physician about documentation prior to patient discharge.
C) assigning codes to the highest degree of specificity documented in the medical record.
D) following software prompts to add CC codes or MCC codes to obtain maximum reimbursement without ensuring corresponding, supporting documentation.
A) re-reviewing documentation after initial coding to search for a CC code or MCC code.
B) performing concurrent coding and questioning the physician about documentation prior to patient discharge.
C) assigning codes to the highest degree of specificity documented in the medical record.
D) following software prompts to add CC codes or MCC codes to obtain maximum reimbursement without ensuring corresponding, supporting documentation.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
43
You are an auditor reviewing a spreadsheet that shows all of the records for the year in which the patient was on a mechanical ventilator. You are reviewing these records because, in every case, the coder has assigned a procedure code indicating that the patient was on mechanical ventilation for over 96 hours. When queried, the coder remarked that the hospital gets a higher reimbursement for that code than for a lower number of hours. You should:
A) accept the coder's explanation, because it is up to the coder to decide what codes to assign to a case.
B) discuss the finding with the Health Information Management Director as a potential abuse or fraud issue.
C) change some of the procedure codes so at least some of them are under 96 hours.
D) ask the coder to re-review all of the records.
A) accept the coder's explanation, because it is up to the coder to decide what codes to assign to a case.
B) discuss the finding with the Health Information Management Director as a potential abuse or fraud issue.
C) change some of the procedure codes so at least some of them are under 96 hours.
D) ask the coder to re-review all of the records.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
44
The clinical documentation improvement specialist works to improve the specificity of patient documentation:
A) before the patient is admitted
B) during the patient's stay
C) after discharge
D) after a claim is denied
A) before the patient is admitted
B) during the patient's stay
C) after discharge
D) after a claim is denied

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
45
In which case would a CDI physician champion be involved?
A) a provider and a clinical documentation improvement specialist disagree on what should be included in the plan of care
B) a nurse is slow to input progress notes
C) a coder adds complications and comorbidities that are unsupported by documentation
D) a provider will not authenticate his verbal orders in a timely manner
A) a provider and a clinical documentation improvement specialist disagree on what should be included in the plan of care
B) a nurse is slow to input progress notes
C) a coder adds complications and comorbidities that are unsupported by documentation
D) a provider will not authenticate his verbal orders in a timely manner

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
46
Structured communication between a clinical documentation improvement (CDI) specialist and a physician is a
A) case mix
B) query
C) E/M code
D) coding compliance plan
A) case mix
B) query
C) E/M code
D) coding compliance plan

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
47
Which is an appropriate measure of the success of a clinical documentation improvement (CDI) program?
A) a more complex case mix
B) higher reimbursements
C) shorter average length of stay
D) diagnosis documentation changes
A) a more complex case mix
B) higher reimbursements
C) shorter average length of stay
D) diagnosis documentation changes

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
48
Coding is the assignment of numeric or _____________ values to diagnosis and procedure descriptions.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
49
The law commonly known as ___________________ names standards for transactions and code sets, which are national standards for exchanging health information electronically.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
50
Level _____________ of HCPCS is also known as Current Procedural Terminology (CPT).

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
51
CMS publishes non-patient-identifiable data compiled to provide information about a group called ____________ data that can be used to compare hospital performance.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
52
DSM-5 diagnoses are coded using the ICD-10- _______________ code set.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
53
The strength, dosage, and formulation of the drug are indicated by the ____________ code, the second segment of the NDC.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck
54
The I- ________________ algorithm maps SNOMED CT codes to the more specific ICD-10-CM code set.

Unlock Deck
Unlock for access to all 54 flashcards in this deck.
Unlock Deck
k this deck


