Deck 14: Anesthesia
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/6
Play
Full screen (f)
Deck 14: Anesthesia
1
AUDIT REPORT T14.2 OPERATIVE REPORT, LAMINOTOMIES
AND FORAMINOTOMIES
The physical status is 1. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
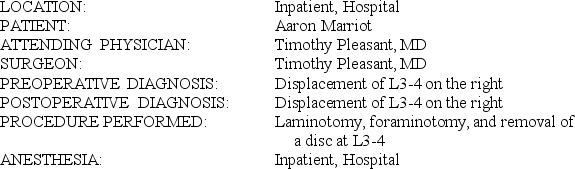 PREOP NOTE: This patient has been counseled regarding his disc, regarding the inability to relieve his pain, the necessity for further surgery, fusion, the complications of persistent pain, pseudomeningocele, and infection. He consents to go ahead with surgery because of the intractable pain.
PREOP NOTE: This patient has been counseled regarding his disc, regarding the inability to relieve his pain, the necessity for further surgery, fusion, the complications of persistent pain, pseudomeningocele, and infection. He consents to go ahead with surgery because of the intractable pain.
DESCRIPTION OF PROCEDURE: Under general anesthesia the patient was placed in prone position. The back was prepped and draped in the usual manner. An incision was made in the skin extending through the subcutaneous tissue, lumbdorsal fascia divided. The erector spini muscles were bluntly dissected from the lamina of L3-4, the interspace was localized via x-ray. I then performed a generous laminotomy, foraminotomy and looked at the L3-4 disc space laterally. There was a hole in the annulus. We entered the disc space and then removed much degenerating material medially and laterally, took it down with curets, took it down with various pituitary rongeurs, and cleaned out the disc space. Irrigated the wound well. Then closed the wound in layers utilizing double-knotted 0 chromic on the lumbdorsal fascia with O Vicryl and 2-0 plain in the subcutaneous tissue and surgical staples on the skin and dressing was applied. The patient was discharged to the recovery room.
One of the following modifiers is incorrectly reported for this case. Indicate the modifier that is incorrect.
T14.2:
PHYSICIAN CODE: 00630-QY-P1_______________________________________
CRNA CODE: 00630-QX-P1____________________________________________
INCORRECT MODIFIER: ______________________________________________
AND FORAMINOTOMIES
The physical status is 1. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
 PREOP NOTE: This patient has been counseled regarding his disc, regarding the inability to relieve his pain, the necessity for further surgery, fusion, the complications of persistent pain, pseudomeningocele, and infection. He consents to go ahead with surgery because of the intractable pain.
PREOP NOTE: This patient has been counseled regarding his disc, regarding the inability to relieve his pain, the necessity for further surgery, fusion, the complications of persistent pain, pseudomeningocele, and infection. He consents to go ahead with surgery because of the intractable pain.DESCRIPTION OF PROCEDURE: Under general anesthesia the patient was placed in prone position. The back was prepped and draped in the usual manner. An incision was made in the skin extending through the subcutaneous tissue, lumbdorsal fascia divided. The erector spini muscles were bluntly dissected from the lamina of L3-4, the interspace was localized via x-ray. I then performed a generous laminotomy, foraminotomy and looked at the L3-4 disc space laterally. There was a hole in the annulus. We entered the disc space and then removed much degenerating material medially and laterally, took it down with curets, took it down with various pituitary rongeurs, and cleaned out the disc space. Irrigated the wound well. Then closed the wound in layers utilizing double-knotted 0 chromic on the lumbdorsal fascia with O Vicryl and 2-0 plain in the subcutaneous tissue and surgical staples on the skin and dressing was applied. The patient was discharged to the recovery room.
One of the following modifiers is incorrectly reported for this case. Indicate the modifier that is incorrect.
T14.2:
PHYSICIAN CODE: 00630-QY-P1_______________________________________
CRNA CODE: 00630-QX-P1____________________________________________
INCORRECT MODIFIER: ______________________________________________
AUDIT REPORT T14.2 OPERATIVE REPORT, LAMINOTOMIES
AND FORAMINOTOMIES
Incorrect modifier: -QY
AND FORAMINOTOMIES
Incorrect modifier: -QY
2
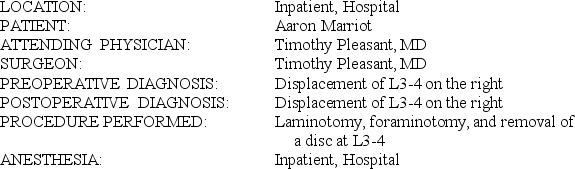
T14-1B OPERATIVE REPORT, ANESTHESIA
This patient has diabetes mellitus that is well controlled with oral insulin. Do not assign diagnosis codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
 This case was monitored with EEG (electroencephalogram). There were some depressions when we clamped, but these returned to normal after reestablishing circulation.
This case was monitored with EEG (electroencephalogram). There were some depressions when we clamped, but these returned to normal after reestablishing circulation.
ANESTHESIA: General
DESCRIPTION OF PROCEDURE: Under general anesthesia, this 82-year-old patient's right side of neck was prepped and draped in the usual manner. An incision was made across the medial border of the sternocleidomastoid. The platysma was divided. The common carotid artery was localized. We put a LigaLoop around it, and then we isolated the external and internal carotid arteries and put LigaLoops around them. We saw the hypoglossal nerve. We put the retractors in and retracted on the upper end of the wound, and then we gave the patient heparin and proceeded with the arteriotomy.
After placing clamps on the internal, common, and external carotid arteries, the arteriotomy was done. There was a severe stenosing atherosclerotic plaque. This was removed. We then sutured the artery up with a 5-0 Prolene at the distal and then at the proximal and meeting in the middle, producing back bleeding and then closing the artery. The wound was then closed in layers after placing a Hemovac in the wound. The wound was approximated with 2-0 chromic, 2-0 plain, and surgical staples on the skin. A dressing was applied. The patient was discharged to recovery.
T14-1B:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
QUALIFYING CIRCUMSTANCES CODE: ___________________
This patient has diabetes mellitus that is well controlled with oral insulin. Do not assign diagnosis codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
 This case was monitored with EEG (electroencephalogram). There were some depressions when we clamped, but these returned to normal after reestablishing circulation.
This case was monitored with EEG (electroencephalogram). There were some depressions when we clamped, but these returned to normal after reestablishing circulation.ANESTHESIA: General
DESCRIPTION OF PROCEDURE: Under general anesthesia, this 82-year-old patient's right side of neck was prepped and draped in the usual manner. An incision was made across the medial border of the sternocleidomastoid. The platysma was divided. The common carotid artery was localized. We put a LigaLoop around it, and then we isolated the external and internal carotid arteries and put LigaLoops around them. We saw the hypoglossal nerve. We put the retractors in and retracted on the upper end of the wound, and then we gave the patient heparin and proceeded with the arteriotomy.
After placing clamps on the internal, common, and external carotid arteries, the arteriotomy was done. There was a severe stenosing atherosclerotic plaque. This was removed. We then sutured the artery up with a 5-0 Prolene at the distal and then at the proximal and meeting in the middle, producing back bleeding and then closing the artery. The wound was then closed in layers after placing a Hemovac in the wound. The wound was approximated with 2-0 chromic, 2-0 plain, and surgical staples on the skin. A dressing was applied. The patient was discharged to recovery.
T14-1B:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
QUALIFYING CIRCUMSTANCES CODE: ___________________
Professional Services:
PHYSICIAN CODE: 00350-QK-P2 (Anesthesia, Neck)
CRNA CODE: 00350-QX-P2 (Anesthesia, Neck)
QUALIFYING CIRCUMSTANCES CODE: 99100 (Anesthesia, Special Circumstances, Extreme Age)
PHYSICIAN CODE: 00350-QK-P2 (Anesthesia, Neck)
CRNA CODE: 00350-QX-P2 (Anesthesia, Neck)
QUALIFYING CIRCUMSTANCES CODE: 99100 (Anesthesia, Special Circumstances, Extreme Age)
3
T14-2B OPERATIVE REPORT, CHOLECYSTECTOMY
Do not assign diagnostic codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
![T14-2B OPERATIVE REPORT, CHOLECYSTECTOMY Do not assign diagnostic codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases. INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed. PROCEDURE: The patient was brought to the operating table and placed under general anesthesia. Foley catheter and orogastric tubes were inserted, and she was prepped and draped sterilely. A supraumbilical skin incision was made with a #11 blade, and dissection was carried down through subcutaneous tissues. Bluntly, midline fascia was grasped with a Kocher clamp, and 0 Vicryl sutures were placed on either side of the midline fascia. The Veress needle was then inserted into the abdominal cavity; drop test confirmed placement within the peritoneal space. The abdomen was insufflated with carbon dioxide; a 10-mm (millimeter) trocar port and laparoscope were introduced, showing no damage to the underlying viscera. Under direct vision, three additional trocar ports were placed, one upper midline 10 mm, two right upper quadrant 5 mm. The gallbladder was grasped and was elevated from its fossa. The cystic duct and artery were dissected and doubly clipped proximally and distally, dividing them with the scissors. The gallbladder was then shelled from its fossa using electrocautery and brought up and out of the upper midline incision. The abdomen was irrigated with saline until returns were clear. There was no bleeding from the liver bed. Clips were in with no evidence of bleeding. When we were removing the final port, we could see down in the right groin, and she had small indirect inguinal hernia, which was about 3 mm in size. We removed the remaining trocar port with no evidence of bleeding, closed the supraumbilical and upper midline ports and fascial defects with interrupted 0 Vicryl sutures, and closed the skin at all port sites with subcuticular 4-0 undyed Vicryl. Steri-Strips and sterile bandages were applied. PATHOLOGY REPORT LATER INDICATED: Benign tissue. T14-2B: PHYSICIAN CODE: ___________________ CRNA CODE: ___________________ QUALIFYING CIRCUMSTANCES CODE: __________________](https://storage.examlex.com/TB6048/11eaa494_d29d_bfb8_9e4a_e5969cc97938_TB6048_00.jpg) INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed.
INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed.
PROCEDURE: The patient was brought to the operating table and placed under general anesthesia. Foley catheter and orogastric tubes were inserted, and she was prepped and draped sterilely. A supraumbilical skin incision was made with a #11 blade, and dissection was carried down through subcutaneous tissues. Bluntly, midline fascia was grasped with a Kocher clamp, and 0 Vicryl sutures were placed on either side of the midline fascia. The Veress needle was then inserted into the abdominal cavity; drop test confirmed placement within the peritoneal space. The abdomen was insufflated with carbon dioxide; a 10-mm (millimeter) trocar port and laparoscope were introduced, showing no damage to the underlying viscera. Under direct vision, three additional trocar ports were placed, one upper midline 10 mm, two right upper quadrant 5 mm. The gallbladder was grasped and was elevated from its fossa. The cystic duct and artery were dissected and doubly clipped proximally and distally, dividing them with the scissors. The gallbladder was then shelled from its fossa using electrocautery and brought up and out of the upper midline incision. The abdomen was irrigated with saline until returns were clear. There was no bleeding from the liver bed. Clips were in with no evidence of bleeding. When we were removing the final port, we could see down in the right groin, and she had small indirect inguinal hernia, which was about 3 mm in size. We removed the remaining trocar port with no evidence of bleeding, closed the supraumbilical and upper midline ports and fascial defects with interrupted 0 Vicryl sutures, and closed the skin at all port sites with subcuticular 4-0 undyed Vicryl. Steri-Strips and sterile bandages were applied.
PATHOLOGY REPORT LATER INDICATED: Benign tissue.
T14-2B:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
QUALIFYING CIRCUMSTANCES CODE: __________________
Do not assign diagnostic codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
![T14-2B OPERATIVE REPORT, CHOLECYSTECTOMY Do not assign diagnostic codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases. INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed. PROCEDURE: The patient was brought to the operating table and placed under general anesthesia. Foley catheter and orogastric tubes were inserted, and she was prepped and draped sterilely. A supraumbilical skin incision was made with a #11 blade, and dissection was carried down through subcutaneous tissues. Bluntly, midline fascia was grasped with a Kocher clamp, and 0 Vicryl sutures were placed on either side of the midline fascia. The Veress needle was then inserted into the abdominal cavity; drop test confirmed placement within the peritoneal space. The abdomen was insufflated with carbon dioxide; a 10-mm (millimeter) trocar port and laparoscope were introduced, showing no damage to the underlying viscera. Under direct vision, three additional trocar ports were placed, one upper midline 10 mm, two right upper quadrant 5 mm. The gallbladder was grasped and was elevated from its fossa. The cystic duct and artery were dissected and doubly clipped proximally and distally, dividing them with the scissors. The gallbladder was then shelled from its fossa using electrocautery and brought up and out of the upper midline incision. The abdomen was irrigated with saline until returns were clear. There was no bleeding from the liver bed. Clips were in with no evidence of bleeding. When we were removing the final port, we could see down in the right groin, and she had small indirect inguinal hernia, which was about 3 mm in size. We removed the remaining trocar port with no evidence of bleeding, closed the supraumbilical and upper midline ports and fascial defects with interrupted 0 Vicryl sutures, and closed the skin at all port sites with subcuticular 4-0 undyed Vicryl. Steri-Strips and sterile bandages were applied. PATHOLOGY REPORT LATER INDICATED: Benign tissue. T14-2B: PHYSICIAN CODE: ___________________ CRNA CODE: ___________________ QUALIFYING CIRCUMSTANCES CODE: __________________](https://storage.examlex.com/TB6048/11eaa494_d29d_bfb8_9e4a_e5969cc97938_TB6048_00.jpg) INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed.
INDICATIONS: The patient is a 78-year-old female who presents with an abnormal CCK (cholecystokinin) HIDA (hepatobiliary imino-diacetic acid [imaging test]) scan. She presents today for elective laparoscopic cholecystectomy. She understands the risks of bleeding, infection, possible damage to the biliary system, and possible conversion to open procedure, and she wishes to proceed.PROCEDURE: The patient was brought to the operating table and placed under general anesthesia. Foley catheter and orogastric tubes were inserted, and she was prepped and draped sterilely. A supraumbilical skin incision was made with a #11 blade, and dissection was carried down through subcutaneous tissues. Bluntly, midline fascia was grasped with a Kocher clamp, and 0 Vicryl sutures were placed on either side of the midline fascia. The Veress needle was then inserted into the abdominal cavity; drop test confirmed placement within the peritoneal space. The abdomen was insufflated with carbon dioxide; a 10-mm (millimeter) trocar port and laparoscope were introduced, showing no damage to the underlying viscera. Under direct vision, three additional trocar ports were placed, one upper midline 10 mm, two right upper quadrant 5 mm. The gallbladder was grasped and was elevated from its fossa. The cystic duct and artery were dissected and doubly clipped proximally and distally, dividing them with the scissors. The gallbladder was then shelled from its fossa using electrocautery and brought up and out of the upper midline incision. The abdomen was irrigated with saline until returns were clear. There was no bleeding from the liver bed. Clips were in with no evidence of bleeding. When we were removing the final port, we could see down in the right groin, and she had small indirect inguinal hernia, which was about 3 mm in size. We removed the remaining trocar port with no evidence of bleeding, closed the supraumbilical and upper midline ports and fascial defects with interrupted 0 Vicryl sutures, and closed the skin at all port sites with subcuticular 4-0 undyed Vicryl. Steri-Strips and sterile bandages were applied.
PATHOLOGY REPORT LATER INDICATED: Benign tissue.
T14-2B:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
QUALIFYING CIRCUMSTANCES CODE: __________________
Professional Services:
PHYSICIAN CODE: 00790-QK-P1 (Anesthesia, Laparoscopy)
CRNA CODE: 00790-QX-P1 (Anesthesia, Laparoscopy)
QUALIFYING CIRCUMSTANCES CODE: 99100 (Anesthesia, Special Circumstances, Extreme Age)
PHYSICIAN CODE: 00790-QK-P1 (Anesthesia, Laparoscopy)
CRNA CODE: 00790-QX-P1 (Anesthesia, Laparoscopy)
QUALIFYING CIRCUMSTANCES CODE: 99100 (Anesthesia, Special Circumstances, Extreme Age)
4
T14-2A OPERATIVE REPORT, ANESTHESIA
The patient has severe systemic disease at the time of the procedure. Do not assign diagnosis codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
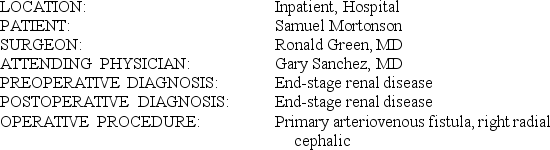 INDICATIONS: This is a 48-year-old man who has end-stage renal disease and is on hemodialysis. He has fair-sized cephalic vein clinically. I discussed with him the primary AV (arteriovenous) fistula between the radial artery and cephalic vein. I had previously discussed this procedure with him. Sometimes, though, veins do not dilate nicely, depending on how many times they have been "poked" for IV (intravenous) access and blood draws. He has been in the hospital a number of times, and so they have had some access to this, but overall clinically it looks pretty good.
INDICATIONS: This is a 48-year-old man who has end-stage renal disease and is on hemodialysis. He has fair-sized cephalic vein clinically. I discussed with him the primary AV (arteriovenous) fistula between the radial artery and cephalic vein. I had previously discussed this procedure with him. Sometimes, though, veins do not dilate nicely, depending on how many times they have been "poked" for IV (intravenous) access and blood draws. He has been in the hospital a number of times, and so they have had some access to this, but overall clinically it looks pretty good.
PROCEDURE: The patient was brought to the operating theater and placed in a supine position on the operating room table. After receiving some IV sedation, he was prepped and draped in a sterile fashion. His cephalic vein was marked out, as was his radial artery. An incision line was marked out halfway between these two. This was longitudinal. It was infiltrated with 0.5% Marcaine with epinephrine. This was left to sit for a couple of minutes. An incision was then made. We dissected out the cephalic vein first. This was done sharply. We were able to get around the circumferential. A couple of small side branches were ligated with 4-0 silks and transected. We were able to dissect up a good segment of the cephalic vein. We then dissected out the radial artery. This was also done sharply. We were able to dissect down to it and dissect it sharply in a circumferential manner. This had a fair amount of calcifications within it. Two very small side branches were taken down with 4-0 silks and transected. We then put a right-angle clamp on the distal aspect of the cephalic vein. It was transected. We ligated this with 2-0 Vicryl. We attached a Titus needle onto the end of the cephalic vein. This dilated up nicely and flushed out quite easily. We then occluded the radial artery proximally and distally with mini vessel loops in a Potts loop fashion. Arteriotomy was made. There was still bleeding coming distally. This was controlled with a small profunda clamp. This worked well. We then irrigated it out with a heparinized saline both proximally and distally for heparinization. We spatulated the end of the vein and cut it to a length. We then performed an end-to-side anastomosis using Gore-Tex CV-7 suture. Prior to placing the last couple of bites, we back-bled and forward-bled and flushed everything out with heparinized saline. We placed the last couple of suture bites and secured our suture line. We opened up the vein and then the proximal radial artery. We let the flow initially go through this and into the vein. We then opened up the distal radial artery. A light thrill was present. With the Doppler, pulses were heard of the radial artery on the wrist distally to our anastomosis as well as on the ulnar artery. The palmar arch also had good flow both proximal and distal. There was distal artery flow and good capsular refill in all fingers. There was good, long diastolic flow through the cephalic vein up the forearm. There was a light thrill present over the area. A good bruit was also audible with a sterile stethoscope. Hemostasis was present. We closed the subcutaneous tissue with 3-0 Vicryl in interrupted fashion. The skin was closed with 4-0 Vicryl in a running subcuticular fashion. Sterile dressings of Telfa and Tegaderm were applied. The patient tolerated the procedure well and went to the recovery room in stable condition.
T14-2A:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
The patient has severe systemic disease at the time of the procedure. Do not assign diagnosis codes. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
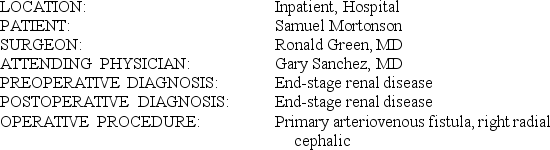 INDICATIONS: This is a 48-year-old man who has end-stage renal disease and is on hemodialysis. He has fair-sized cephalic vein clinically. I discussed with him the primary AV (arteriovenous) fistula between the radial artery and cephalic vein. I had previously discussed this procedure with him. Sometimes, though, veins do not dilate nicely, depending on how many times they have been "poked" for IV (intravenous) access and blood draws. He has been in the hospital a number of times, and so they have had some access to this, but overall clinically it looks pretty good.
INDICATIONS: This is a 48-year-old man who has end-stage renal disease and is on hemodialysis. He has fair-sized cephalic vein clinically. I discussed with him the primary AV (arteriovenous) fistula between the radial artery and cephalic vein. I had previously discussed this procedure with him. Sometimes, though, veins do not dilate nicely, depending on how many times they have been "poked" for IV (intravenous) access and blood draws. He has been in the hospital a number of times, and so they have had some access to this, but overall clinically it looks pretty good.PROCEDURE: The patient was brought to the operating theater and placed in a supine position on the operating room table. After receiving some IV sedation, he was prepped and draped in a sterile fashion. His cephalic vein was marked out, as was his radial artery. An incision line was marked out halfway between these two. This was longitudinal. It was infiltrated with 0.5% Marcaine with epinephrine. This was left to sit for a couple of minutes. An incision was then made. We dissected out the cephalic vein first. This was done sharply. We were able to get around the circumferential. A couple of small side branches were ligated with 4-0 silks and transected. We were able to dissect up a good segment of the cephalic vein. We then dissected out the radial artery. This was also done sharply. We were able to dissect down to it and dissect it sharply in a circumferential manner. This had a fair amount of calcifications within it. Two very small side branches were taken down with 4-0 silks and transected. We then put a right-angle clamp on the distal aspect of the cephalic vein. It was transected. We ligated this with 2-0 Vicryl. We attached a Titus needle onto the end of the cephalic vein. This dilated up nicely and flushed out quite easily. We then occluded the radial artery proximally and distally with mini vessel loops in a Potts loop fashion. Arteriotomy was made. There was still bleeding coming distally. This was controlled with a small profunda clamp. This worked well. We then irrigated it out with a heparinized saline both proximally and distally for heparinization. We spatulated the end of the vein and cut it to a length. We then performed an end-to-side anastomosis using Gore-Tex CV-7 suture. Prior to placing the last couple of bites, we back-bled and forward-bled and flushed everything out with heparinized saline. We placed the last couple of suture bites and secured our suture line. We opened up the vein and then the proximal radial artery. We let the flow initially go through this and into the vein. We then opened up the distal radial artery. A light thrill was present. With the Doppler, pulses were heard of the radial artery on the wrist distally to our anastomosis as well as on the ulnar artery. The palmar arch also had good flow both proximal and distal. There was distal artery flow and good capsular refill in all fingers. There was good, long diastolic flow through the cephalic vein up the forearm. There was a light thrill present over the area. A good bruit was also audible with a sterile stethoscope. Hemostasis was present. We closed the subcutaneous tissue with 3-0 Vicryl in interrupted fashion. The skin was closed with 4-0 Vicryl in a running subcuticular fashion. Sterile dressings of Telfa and Tegaderm were applied. The patient tolerated the procedure well and went to the recovery room in stable condition.
T14-2A:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
5
AUDIT REPORT T14.1 OPERATIVE REPORT, RESECTION
HEMANGIOMA
This anesthesia service is being provided for a 78-year old patient. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 3 concurrent cases. The physical status is 2.
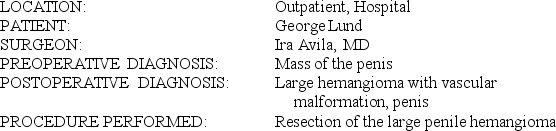 CLINICAL NOTE: This is a 89-year-old man who presents with a 2-month history of pain on the dorsal penile area. Ultrasound showed this to be a solid mass. No flow was seen within it. It is thought to possibly be a sarcoma. It is a soft mass, and it may be vascular. Resection will be done to determine what we are dealing with.
CLINICAL NOTE: This is a 89-year-old man who presents with a 2-month history of pain on the dorsal penile area. Ultrasound showed this to be a solid mass. No flow was seen within it. It is thought to possibly be a sarcoma. It is a soft mass, and it may be vascular. Resection will be done to determine what we are dealing with.
OPERATIVE NOTE: The patient was placed under general anesthesia via endotracheal tube. The patient was prepped and draped in the supine position. An incision was made on the dorsal side of the penile shaft, overlying the mass. Just below the skin, a large vein was encountered. Bleeding was controlled with ligation using 3-0 chromic ligatures. The mass was seen and was approximately 9 cm long. Under closer inspection this was noted to be a hemangioma coming from the superficial veins from Buck's fascia. Care and mobilization were taken, and all perforating vessels were individually ligated with chromic ligature. Photographs were taken during the procedure showing the extreme vascularity of the lesion. Frozen section was taken, and this showed no malignancy present. After the mass was resected it left a large cavity in the base of the patient's penile shaft. The subcutaneous tissues were closed with 4-0 chromic, and the skin was closed with subcuticular Dexon. A compression dressing was applied. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
PATHOLOGY REPORT LATER INDICATED: Benign hemangioma
One of the following modifiers is incorrectly reported for this case. Indicate the modifier that is incorrect.
T14.1:
PHYSICIAN CODE: 00920-QY-P2, 99100_______________
CRNA CODE: 00920-QX-P2__________________________
INCORRECT MODIFIER:___________________________
HEMANGIOMA
This anesthesia service is being provided for a 78-year old patient. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 3 concurrent cases. The physical status is 2.
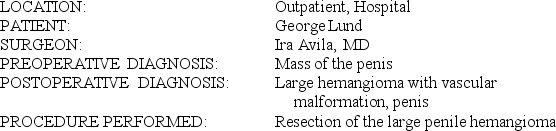 CLINICAL NOTE: This is a 89-year-old man who presents with a 2-month history of pain on the dorsal penile area. Ultrasound showed this to be a solid mass. No flow was seen within it. It is thought to possibly be a sarcoma. It is a soft mass, and it may be vascular. Resection will be done to determine what we are dealing with.
CLINICAL NOTE: This is a 89-year-old man who presents with a 2-month history of pain on the dorsal penile area. Ultrasound showed this to be a solid mass. No flow was seen within it. It is thought to possibly be a sarcoma. It is a soft mass, and it may be vascular. Resection will be done to determine what we are dealing with.OPERATIVE NOTE: The patient was placed under general anesthesia via endotracheal tube. The patient was prepped and draped in the supine position. An incision was made on the dorsal side of the penile shaft, overlying the mass. Just below the skin, a large vein was encountered. Bleeding was controlled with ligation using 3-0 chromic ligatures. The mass was seen and was approximately 9 cm long. Under closer inspection this was noted to be a hemangioma coming from the superficial veins from Buck's fascia. Care and mobilization were taken, and all perforating vessels were individually ligated with chromic ligature. Photographs were taken during the procedure showing the extreme vascularity of the lesion. Frozen section was taken, and this showed no malignancy present. After the mass was resected it left a large cavity in the base of the patient's penile shaft. The subcutaneous tissues were closed with 4-0 chromic, and the skin was closed with subcuticular Dexon. A compression dressing was applied. The patient tolerated the procedure well and was transferred to the recovery room in stable condition.
PATHOLOGY REPORT LATER INDICATED: Benign hemangioma
One of the following modifiers is incorrectly reported for this case. Indicate the modifier that is incorrect.
T14.1:
PHYSICIAN CODE: 00920-QY-P2, 99100_______________
CRNA CODE: 00920-QX-P2__________________________
INCORRECT MODIFIER:___________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
6
T14-1A OPERATIVE REPORT, ANESTHESIA
This patient is a healthy, 42-year-old patient except for the subdural hematoma. Do not assign diagnosis codes. Ventriculography was not used during the procedure. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
 PROCEDURE: Under general anesthesia, the left side of head was prepped and draped in the usual manner, after having been placed in Mayfield pins. Hemoclips and Dandy clips were utilized on the scalp edges. Part of the temporalis muscle was taken down. Two burr holes were made, and a circumferential flap was made. The bone was elevated. The dura was incised in an inverted U-shaped fashion. We saw acute clot; probably 45-50 cc (cubic centimeter) of clot was irrigated from the frontal, temporal, and posterior parietal areas. Having cleaned it out, there was no free bleeder that I saw. I placed a piece of Gelfoam on the brain and then began closure of the dura with 3-0 Vicryl; this was done. A little patch was necessary; we used temporalis fascia. We tacked up the dura, replaced the bone flap, and utilized Wurzburg plates and burr hole cover. Having secured this, we then closed the scalp with 2-0 Vicryl on the galea with surgical staples on the skin, with a Hemovac drain having been applied prior to closure.
PROCEDURE: Under general anesthesia, the left side of head was prepped and draped in the usual manner, after having been placed in Mayfield pins. Hemoclips and Dandy clips were utilized on the scalp edges. Part of the temporalis muscle was taken down. Two burr holes were made, and a circumferential flap was made. The bone was elevated. The dura was incised in an inverted U-shaped fashion. We saw acute clot; probably 45-50 cc (cubic centimeter) of clot was irrigated from the frontal, temporal, and posterior parietal areas. Having cleaned it out, there was no free bleeder that I saw. I placed a piece of Gelfoam on the brain and then began closure of the dura with 3-0 Vicryl; this was done. A little patch was necessary; we used temporalis fascia. We tacked up the dura, replaced the bone flap, and utilized Wurzburg plates and burr hole cover. Having secured this, we then closed the scalp with 2-0 Vicryl on the galea with surgical staples on the skin, with a Hemovac drain having been applied prior to closure.
T14-1A:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________
This patient is a healthy, 42-year-old patient except for the subdural hematoma. Do not assign diagnosis codes. Ventriculography was not used during the procedure. Anesthesia by: MDA and CRNA. Anesthesiologist was medically directing 4 concurrent cases.
 PROCEDURE: Under general anesthesia, the left side of head was prepped and draped in the usual manner, after having been placed in Mayfield pins. Hemoclips and Dandy clips were utilized on the scalp edges. Part of the temporalis muscle was taken down. Two burr holes were made, and a circumferential flap was made. The bone was elevated. The dura was incised in an inverted U-shaped fashion. We saw acute clot; probably 45-50 cc (cubic centimeter) of clot was irrigated from the frontal, temporal, and posterior parietal areas. Having cleaned it out, there was no free bleeder that I saw. I placed a piece of Gelfoam on the brain and then began closure of the dura with 3-0 Vicryl; this was done. A little patch was necessary; we used temporalis fascia. We tacked up the dura, replaced the bone flap, and utilized Wurzburg plates and burr hole cover. Having secured this, we then closed the scalp with 2-0 Vicryl on the galea with surgical staples on the skin, with a Hemovac drain having been applied prior to closure.
PROCEDURE: Under general anesthesia, the left side of head was prepped and draped in the usual manner, after having been placed in Mayfield pins. Hemoclips and Dandy clips were utilized on the scalp edges. Part of the temporalis muscle was taken down. Two burr holes were made, and a circumferential flap was made. The bone was elevated. The dura was incised in an inverted U-shaped fashion. We saw acute clot; probably 45-50 cc (cubic centimeter) of clot was irrigated from the frontal, temporal, and posterior parietal areas. Having cleaned it out, there was no free bleeder that I saw. I placed a piece of Gelfoam on the brain and then began closure of the dura with 3-0 Vicryl; this was done. A little patch was necessary; we used temporalis fascia. We tacked up the dura, replaced the bone flap, and utilized Wurzburg plates and burr hole cover. Having secured this, we then closed the scalp with 2-0 Vicryl on the galea with surgical staples on the skin, with a Hemovac drain having been applied prior to closure.T14-1A:
PHYSICIAN CODE: ___________________
CRNA CODE: ___________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck


