Deck 2: Medicine
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/6
Play
Full screen (f)
Deck 2: Medicine
1
AUDIT REPORT T2.1 PHYSICAL THERAPY EVALUATION
The following is an initial physical therapy evaluation for which you are to report Mary Barneswell's service.
 SUBJECTIVE: Michelle is a female patient seen in Hand Therapy on direct referral from Dr. Ronald Green with the above diagnosis. This is a patient that was diagnosed with breast cancer a year ago. She currently is undergoing active chemotherapy treatments. She had surgery a year ago and had no edema until the past month. She is also complaining of some shoulder discomfort in the right.
SUBJECTIVE: Michelle is a female patient seen in Hand Therapy on direct referral from Dr. Ronald Green with the above diagnosis. This is a patient that was diagnosed with breast cancer a year ago. She currently is undergoing active chemotherapy treatments. She had surgery a year ago and had no edema until the past month. She is also complaining of some shoulder discomfort in the right.
OBJECTIVE: The patient presents today with a right upper extremity that has some areas of red, blotchy skin with some slight increase in edema through the entire arm. Patient indicates that at times the red areas in her arm are fairly bright red and inflamed looking. She notes that the swelling is somewhat down today compared to other days.
Circumferential measurements taken today are as follows: On the right, the metacarpals are 20 cm, wrist 17.5 cm, 9 cm above the wrist 21.3 cm, 16 cm above the wrist 23.7 cm, elbow 27 cm, 12 cm above the elbow 33 cm, and axilla 35 cm. On the left, the metacarpals 18.5 cm, wrist 17 cm, 9 cm above the wrist 19.8 cm, 16 cm above the wrist 23 cm, elbow 25.2 cm, 12 cm above the elbow 30.2, and axilla 35 cm.
The patient has not had any hand or thumb swelling to speak of, and fingers look comparable to the noninvolved left side. She has no numbness or tingling but does complain of some shoulder discomfort. Active range of motion in the right upper extremity is full, with exception of end ranges of shoulder motion lacking 20 for flexion and extension.
DIRECT TREATMENT: The patient is seen today primarily for the fitting of a sleeve per physician's orders. Today we fitted her with an over-the-counter size VI Juzo sleeve. Fit was fairly good today. The patient was instructed to wear this sleeve during daytime activities and to remove it overnight. She is able to independently apply it. She was also sent with a tube of roll-on grip to utilize on her skin to help hold the sleeve in a good position on her arm. We then reviewed some gentle massage techniques focusing on moving the fluid up, out of the arm and towards the shoulder area. The patient was able to understand these and could complete these a couple times per day. We also reviewed some general lymphedema precautions as well as skin care.
ASSESSMENT: Lymphedema and arm swelling.
PLAN: This patient is not in need of direct ongoing care. I am hopeful that with the use of her over-the-counter sleeve, her swelling will be well controlled. The patient's long-term goals are to achieve maintenance of decrease in the swelling in her arm and be able to use her arm unrestricted for all tasks. Short-term goals include pain-free use of her arm for all activities, including use of her crutch at home, no increase in swelling during the daytime with the use of the sleeve, continued assessment of the edema and the skin condition with progression to a more active massage program or bandaging if the need arises.
The patient was given a phone number and a card and instructed to phone us if things flare or if she is not doing well with the use of her sleeve.
T2.1:
SERVICE CODE(S): 97162____________________________________________
ICD-10-CM DX CODE(S): I97.2________________________________________
INCORRECT/MISSING CODE(S): _____________________________________
The following is an initial physical therapy evaluation for which you are to report Mary Barneswell's service.
 SUBJECTIVE: Michelle is a female patient seen in Hand Therapy on direct referral from Dr. Ronald Green with the above diagnosis. This is a patient that was diagnosed with breast cancer a year ago. She currently is undergoing active chemotherapy treatments. She had surgery a year ago and had no edema until the past month. She is also complaining of some shoulder discomfort in the right.
SUBJECTIVE: Michelle is a female patient seen in Hand Therapy on direct referral from Dr. Ronald Green with the above diagnosis. This is a patient that was diagnosed with breast cancer a year ago. She currently is undergoing active chemotherapy treatments. She had surgery a year ago and had no edema until the past month. She is also complaining of some shoulder discomfort in the right.OBJECTIVE: The patient presents today with a right upper extremity that has some areas of red, blotchy skin with some slight increase in edema through the entire arm. Patient indicates that at times the red areas in her arm are fairly bright red and inflamed looking. She notes that the swelling is somewhat down today compared to other days.
Circumferential measurements taken today are as follows: On the right, the metacarpals are 20 cm, wrist 17.5 cm, 9 cm above the wrist 21.3 cm, 16 cm above the wrist 23.7 cm, elbow 27 cm, 12 cm above the elbow 33 cm, and axilla 35 cm. On the left, the metacarpals 18.5 cm, wrist 17 cm, 9 cm above the wrist 19.8 cm, 16 cm above the wrist 23 cm, elbow 25.2 cm, 12 cm above the elbow 30.2, and axilla 35 cm.
The patient has not had any hand or thumb swelling to speak of, and fingers look comparable to the noninvolved left side. She has no numbness or tingling but does complain of some shoulder discomfort. Active range of motion in the right upper extremity is full, with exception of end ranges of shoulder motion lacking 20 for flexion and extension.
DIRECT TREATMENT: The patient is seen today primarily for the fitting of a sleeve per physician's orders. Today we fitted her with an over-the-counter size VI Juzo sleeve. Fit was fairly good today. The patient was instructed to wear this sleeve during daytime activities and to remove it overnight. She is able to independently apply it. She was also sent with a tube of roll-on grip to utilize on her skin to help hold the sleeve in a good position on her arm. We then reviewed some gentle massage techniques focusing on moving the fluid up, out of the arm and towards the shoulder area. The patient was able to understand these and could complete these a couple times per day. We also reviewed some general lymphedema precautions as well as skin care.
ASSESSMENT: Lymphedema and arm swelling.
PLAN: This patient is not in need of direct ongoing care. I am hopeful that with the use of her over-the-counter sleeve, her swelling will be well controlled. The patient's long-term goals are to achieve maintenance of decrease in the swelling in her arm and be able to use her arm unrestricted for all tasks. Short-term goals include pain-free use of her arm for all activities, including use of her crutch at home, no increase in swelling during the daytime with the use of the sleeve, continued assessment of the edema and the skin condition with progression to a more active massage program or bandaging if the need arises.
The patient was given a phone number and a card and instructed to phone us if things flare or if she is not doing well with the use of her sleeve.
T2.1:
SERVICE CODE(S): 97162____________________________________________
ICD-10-CM DX CODE(S): I97.2________________________________________
INCORRECT/MISSING CODE(S): _____________________________________
INCORRECT/MISSING CODE(S): Z51.89
2
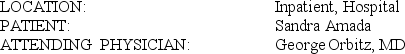
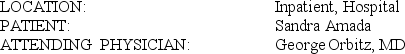
T2-2A HEMODIALYSIS PROGRESS NOTE
 HEMODIALYSIS PROGRESS NOTE: The patient is seen and examined during hemodialysis. The patient appears to be hemodynamically stable, not in any form of respiratory distress or compromise.
HEMODIALYSIS PROGRESS NOTE: The patient is seen and examined during hemodialysis. The patient appears to be hemodynamically stable, not in any form of respiratory distress or compromise.
LABORATORY STUDIES: Latest labs were performed 4 weeks ago. Hemogram shows an H&H (hematocrit and hemoglobin) of 8.6/26.2. WBC (white blood count) is 9.9, normochromic/normocytic indices. Platelets are 143. There is left shift of 81.1% neutrophils. Sodium is 139, potassium 4, chloride 98, CO2 (carbon dioxide) is 30.7, BUN (blood urea nitrogen) and creatinine 31/3.4, glucose 121, and calcium 8.2.
Today, we will dialyze her for a total of 4 hours using an HP-150 dialyzer via her right-sided Perm-A-Cath. We will use a 2.0 potassium bath, and we will not give her any heparin loading dose during this treatment.
PHYSICAL EXAM: At present time, vital signs are stable. Blood pressure is 128/57. Heart rate is 80, and she is tolerating a blood flow rate of 500 ml (milliliter) per minute. Normocephalic and atraumatic. Pale palpebral conjunctivae, anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy. Symmetrical chest. No retractions. Positive rhonchi. No crackles or wheezes. S1 (first heart sound) and S2 (second heart sound) distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. No abdominal bruits. Both upper and lower extremities reveal arthritic changes. Pulses are fair.
ASSESSMENT/PLAN:
1. End-stage renal disease (on maintenance hemodialysis, Monday, Wednesday, and Friday), most likely secondary to the following:
A. Hypertension. Continue same antihypertensive regimen as ordered.
B. Type 2 diabetes mellitus. Continue oral antidiabetic agents. Continue the same dialysis orders as above.
C. Previous chronic use of NSAID (nonsteroidal antiinflammatory drug)/COX-2 inhibitors.
2. Anemia due to chronic renal disease.
3. Questionable diverticulosis; status post multiple herniorrhaphies; status post- cholecystectomy.
4. Discharge planning: The plan is to discharge the patient to rehabilitation medicine.
At this time, the patient appears to be stable and is tolerating hemodialysis. We will continue to follow this patient from the renal/hemodialysis standpoint. She will get erythropoietin 10,000 units IV (intravenous) after hemodialysis today.
T2-2A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
 HEMODIALYSIS PROGRESS NOTE: The patient is seen and examined during hemodialysis. The patient appears to be hemodynamically stable, not in any form of respiratory distress or compromise.
HEMODIALYSIS PROGRESS NOTE: The patient is seen and examined during hemodialysis. The patient appears to be hemodynamically stable, not in any form of respiratory distress or compromise.LABORATORY STUDIES: Latest labs were performed 4 weeks ago. Hemogram shows an H&H (hematocrit and hemoglobin) of 8.6/26.2. WBC (white blood count) is 9.9, normochromic/normocytic indices. Platelets are 143. There is left shift of 81.1% neutrophils. Sodium is 139, potassium 4, chloride 98, CO2 (carbon dioxide) is 30.7, BUN (blood urea nitrogen) and creatinine 31/3.4, glucose 121, and calcium 8.2.
Today, we will dialyze her for a total of 4 hours using an HP-150 dialyzer via her right-sided Perm-A-Cath. We will use a 2.0 potassium bath, and we will not give her any heparin loading dose during this treatment.
PHYSICAL EXAM: At present time, vital signs are stable. Blood pressure is 128/57. Heart rate is 80, and she is tolerating a blood flow rate of 500 ml (milliliter) per minute. Normocephalic and atraumatic. Pale palpebral conjunctivae, anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy. Symmetrical chest. No retractions. Positive rhonchi. No crackles or wheezes. S1 (first heart sound) and S2 (second heart sound) distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. No abdominal bruits. Both upper and lower extremities reveal arthritic changes. Pulses are fair.
ASSESSMENT/PLAN:
1. End-stage renal disease (on maintenance hemodialysis, Monday, Wednesday, and Friday), most likely secondary to the following:
A. Hypertension. Continue same antihypertensive regimen as ordered.
B. Type 2 diabetes mellitus. Continue oral antidiabetic agents. Continue the same dialysis orders as above.
C. Previous chronic use of NSAID (nonsteroidal antiinflammatory drug)/COX-2 inhibitors.
2. Anemia due to chronic renal disease.
3. Questionable diverticulosis; status post multiple herniorrhaphies; status post- cholecystectomy.
4. Discharge planning: The plan is to discharge the patient to rehabilitation medicine.
At this time, the patient appears to be stable and is tolerating hemodialysis. We will continue to follow this patient from the renal/hemodialysis standpoint. She will get erythropoietin 10,000 units IV (intravenous) after hemodialysis today.
T2-2A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Professional Services: 90935 (Hemodialysis)
ICD-10-CM DX: I12.0 (Hypertension/hypertensive, kidney, with stage 5 chronic kidney disease [CKD] or end stage renal disease [ESRD]), N18.6 (Disease/diseased, renal, end-stage), E11.21 (Diabetes/diabetic, with, nephropathy), D63.1 (Anemia, in, end stage renal disease)
ICD-10-CM DX: I12.0 (Hypertension/hypertensive, kidney, with stage 5 chronic kidney disease [CKD] or end stage renal disease [ESRD]), N18.6 (Disease/diseased, renal, end-stage), E11.21 (Diabetes/diabetic, with, nephropathy), D63.1 (Anemia, in, end stage renal disease)
3
T2-2B DISCHARGE SUMMARY
 The patient was admitted primarily because of uremic symptomatology, namely hyperkalemia/bradycardia and generalized weakness.
The patient was admitted primarily because of uremic symptomatology, namely hyperkalemia/bradycardia and generalized weakness.
The patient was admitted because of the aforementioned symptoms. The patient was then taken to ICU (intensive care unit) for emergent hemodialysis. The patient tolerated the dialysis procedure without any problems. The patient has remained hemodynamically stable throughout this hospitalization.
Consultations during this hospitalization including the following: Dr. Elhart of cardiology and Dr. Barneswell of rehabilitation medicine.
EXAMINATION: Vital signs are stable. Blood pressure: 100/46. Heart rate: 76. Respirations: 20. Temperature: 36.68°C (Celsius). Saturating 92% on room air. Normocephalic and atraumatic. Pink palpebral conjunctivae, anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy. Symmetrical chest. S1 (first heart sound) and S2 (second heart sound) are distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. No abdominal bruits. Both upper and lower extremities reveal arthritic changes. Pulses are fair.
DISCHARGE INSTRUCTIONS: Activity level as tolerated. Diet: Renal diabetic diet.
MEDICATIONS:
1. Lipitor 10 mg (milligram) q.d. (every day).
2. Epogen 10,000 units IV (intravenous) every hemodialysis session.
3. Glipizide 10 mg q.d.
4. Levothroid 0.88 mg q.d.
5. Procardia XL 60 mg q.d.
6. Senokot-S 1-4 tabs t.i.d. (three times a day).
FOLLOW-UP APPOINTMENT CARE:
1. The patient is to be followed up during her hemodialysis sessions in the dialysis unit.
2. The patient is to be discharged to rehabilitation medicine under the care of Dr. Barneswell for deconditioning.
CONDITION OF DISCHARGE AS COMPARED TO CONDITION ON ADMISSION: Significantly improved.
FINAL DIAGNOSES:
1. End-stage renal disease on maintenance hemodialysis (Monday, Wednesday, and Friday), secondary to the following:
A. Hypertension.
B. Type 2 diabetes mellitus.
C. Questionable previous chronic use of nonsteroidal antiinflammatory drugs/COX-2 (cyclooxygenase-2) inhibitors.
2. Anemia due to chronic renal failure.
3. Hyperkalemia.
4. Diverticulosis; status post multiple herniorrhaphies; status post cholecystectomy.
PROCEDURES PERFORMED:
1. Hemodialysis sessions.
2. Tunneled hemodialysis central venous catheter placement per Dr. Riddle of interventional radiology on Day 2.
3. Right femoral temporary hemodialysis catheter placement per Dr. Pleasant on Day 3.
I spent a total of 50 minutes evaluating and reviewing this patient's medical record, and I spent an additional 20 minutes discussing the discharge plans with the patient.
T2-2B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
 The patient was admitted primarily because of uremic symptomatology, namely hyperkalemia/bradycardia and generalized weakness.
The patient was admitted primarily because of uremic symptomatology, namely hyperkalemia/bradycardia and generalized weakness.The patient was admitted because of the aforementioned symptoms. The patient was then taken to ICU (intensive care unit) for emergent hemodialysis. The patient tolerated the dialysis procedure without any problems. The patient has remained hemodynamically stable throughout this hospitalization.
Consultations during this hospitalization including the following: Dr. Elhart of cardiology and Dr. Barneswell of rehabilitation medicine.
EXAMINATION: Vital signs are stable. Blood pressure: 100/46. Heart rate: 76. Respirations: 20. Temperature: 36.68°C (Celsius). Saturating 92% on room air. Normocephalic and atraumatic. Pink palpebral conjunctivae, anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy. Symmetrical chest. S1 (first heart sound) and S2 (second heart sound) are distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. No abdominal bruits. Both upper and lower extremities reveal arthritic changes. Pulses are fair.
DISCHARGE INSTRUCTIONS: Activity level as tolerated. Diet: Renal diabetic diet.
MEDICATIONS:
1. Lipitor 10 mg (milligram) q.d. (every day).
2. Epogen 10,000 units IV (intravenous) every hemodialysis session.
3. Glipizide 10 mg q.d.
4. Levothroid 0.88 mg q.d.
5. Procardia XL 60 mg q.d.
6. Senokot-S 1-4 tabs t.i.d. (three times a day).
FOLLOW-UP APPOINTMENT CARE:
1. The patient is to be followed up during her hemodialysis sessions in the dialysis unit.
2. The patient is to be discharged to rehabilitation medicine under the care of Dr. Barneswell for deconditioning.
CONDITION OF DISCHARGE AS COMPARED TO CONDITION ON ADMISSION: Significantly improved.
FINAL DIAGNOSES:
1. End-stage renal disease on maintenance hemodialysis (Monday, Wednesday, and Friday), secondary to the following:
A. Hypertension.
B. Type 2 diabetes mellitus.
C. Questionable previous chronic use of nonsteroidal antiinflammatory drugs/COX-2 (cyclooxygenase-2) inhibitors.
2. Anemia due to chronic renal failure.
3. Hyperkalemia.
4. Diverticulosis; status post multiple herniorrhaphies; status post cholecystectomy.
PROCEDURES PERFORMED:
1. Hemodialysis sessions.
2. Tunneled hemodialysis central venous catheter placement per Dr. Riddle of interventional radiology on Day 2.
3. Right femoral temporary hemodialysis catheter placement per Dr. Pleasant on Day 3.
I spent a total of 50 minutes evaluating and reviewing this patient's medical record, and I spent an additional 20 minutes discussing the discharge plans with the patient.
T2-2B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Professional Services: 99239 (Evaluation and Management, Hospital, Discharge)
ICD-10-CM DX: I12.0 (Hypertension/hypertensive, kidney, with stage 5 chronic kidney disease [CKD] or end stage renal disease [ESRD]), N18.6 (Disease/diseased, renal, end-stage), E11.21 (Diabetes/diabetic, with, nephropathy), D63.1 (Anemia, in, end stage renal disease), E87.5 (Hyperkalemia)
ICD-10-CM DX: I12.0 (Hypertension/hypertensive, kidney, with stage 5 chronic kidney disease [CKD] or end stage renal disease [ESRD]), N18.6 (Disease/diseased, renal, end-stage), E11.21 (Diabetes/diabetic, with, nephropathy), D63.1 (Anemia, in, end stage renal disease), E87.5 (Hyperkalemia)
4
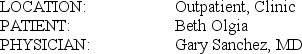
T2-1B CLINIC PROGRESS NOTE
This patient presents to the physician's office for an examination after a C-section the previous week.
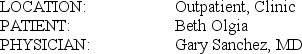 SUBJECTIVE: Beth came in today for a postoperative exam. She underwent a C-section last week along with a tubal ligation. She was discharged on Monday of this week and is back in for a staple removal. Her blood pressure is still up, and today it is 170/102. Dr. Naraquist has been following this. She says her blood sugars have been okay. Dr. Naraquist is following her blood sugars.
SUBJECTIVE: Beth came in today for a postoperative exam. She underwent a C-section last week along with a tubal ligation. She was discharged on Monday of this week and is back in for a staple removal. Her blood pressure is still up, and today it is 170/102. Dr. Naraquist has been following this. She says her blood sugars have been okay. Dr. Naraquist is following her blood sugars.
CURRENT MEDICATIONS:
1. Prenatal vitamins once a day.
2. Peri-Colace 1 b.i.d. (twice a day).
3. Darvocet p.r.n. (as needed).
4. Labetalol 600 mg (milligram) q.a.m. (every morning), 200 mg at 3 PM, and 600 mg at bedtime.
ALLERGIES: None
OBJECTIVE: Her wound is healing okay. The staples are removed. I told her not to do any heavy lifting over 20 pounds for the next 5 weeks, also no intercourse. She is to see us back again in 5 weeks.
T2-1B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): _______________________________________________
This patient presents to the physician's office for an examination after a C-section the previous week.
 SUBJECTIVE: Beth came in today for a postoperative exam. She underwent a C-section last week along with a tubal ligation. She was discharged on Monday of this week and is back in for a staple removal. Her blood pressure is still up, and today it is 170/102. Dr. Naraquist has been following this. She says her blood sugars have been okay. Dr. Naraquist is following her blood sugars.
SUBJECTIVE: Beth came in today for a postoperative exam. She underwent a C-section last week along with a tubal ligation. She was discharged on Monday of this week and is back in for a staple removal. Her blood pressure is still up, and today it is 170/102. Dr. Naraquist has been following this. She says her blood sugars have been okay. Dr. Naraquist is following her blood sugars.CURRENT MEDICATIONS:
1. Prenatal vitamins once a day.
2. Peri-Colace 1 b.i.d. (twice a day).
3. Darvocet p.r.n. (as needed).
4. Labetalol 600 mg (milligram) q.a.m. (every morning), 200 mg at 3 PM, and 600 mg at bedtime.
ALLERGIES: None
OBJECTIVE: Her wound is healing okay. The staples are removed. I told her not to do any heavy lifting over 20 pounds for the next 5 weeks, also no intercourse. She is to see us back again in 5 weeks.
T2-1B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): _______________________________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
5
AUDIT REPORT T2.2 ULTRASOUND, LOWER EXTREMITIES
 ULTRASOUND OF BOTH LOWER EXTREMITIES: FINDINGS: Ultrasound examination of the deep venous system of the lower extremities shows a deep venous thrombosis of the superficial femoral vein of the right leg. Bilateral posterior tibial, greater saphenous, femoral and popliteal veins are patent with no evidence of thrombus seen there.
ULTRASOUND OF BOTH LOWER EXTREMITIES: FINDINGS: Ultrasound examination of the deep venous system of the lower extremities shows a deep venous thrombosis of the superficial femoral vein of the right leg. Bilateral posterior tibial, greater saphenous, femoral and popliteal veins are patent with no evidence of thrombus seen there.
T2.2:
SERVICE CODE(S): 93971-50__________________________________________
ICD-10-CM DX CODE(S): M79.661, M79.662, I82.411______________________
INCORRECT/MISSING CODE(S): _____________________________________
 ULTRASOUND OF BOTH LOWER EXTREMITIES: FINDINGS: Ultrasound examination of the deep venous system of the lower extremities shows a deep venous thrombosis of the superficial femoral vein of the right leg. Bilateral posterior tibial, greater saphenous, femoral and popliteal veins are patent with no evidence of thrombus seen there.
ULTRASOUND OF BOTH LOWER EXTREMITIES: FINDINGS: Ultrasound examination of the deep venous system of the lower extremities shows a deep venous thrombosis of the superficial femoral vein of the right leg. Bilateral posterior tibial, greater saphenous, femoral and popliteal veins are patent with no evidence of thrombus seen there.T2.2:
SERVICE CODE(S): 93971-50__________________________________________
ICD-10-CM DX CODE(S): M79.661, M79.662, I82.411______________________
INCORRECT/MISSING CODE(S): _____________________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
6
T2-1A HEMODIALYSIS PROGRESS REPORT
The patient is seen in the outpatient dialysis unit for the purpose of hemodialysis. Report only the monthly dialysis services of the physician for 4 or more visits during the month.
This 57-year-old patient is seen and examined during hemodialysis. Chart is reviewed. The patient appears to be hemodynamically stable and not in any form of respiratory distress or compromise. She is tolerating dialysis without any problems. Predialysis vital signs are stable. Blood pressure is 134/63, heart rate 57, and temperature 98.6 F. She weighs 139.8 pounds. Today, we will dialyze her using her left Perm-A-Cath for a total of 3 hours using an HP-150 dialyzer and a 2.0 potassium bath. We will give her a Heparin loading dose of 2000 units and then maintenance of 1 ml (milliliter) per hour.
At the present time, vital signs are stable. Blood pressure is 117/61, heart rate 57, and she is tolerating a blood flow rate of 350 mL per minute. Normocephalic and atraumatic. Pale palpebral conjunctivae. Anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy; symmetrical chest. No retractions. Positive rhonchi. No crackles or wheezes. S1 (first heart sound) and S2 (second heart second) distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. Status post below-knee amputation. Pulses are fair.
Latest labs performed 1 month ago are as follows: Sodium 136, potassium 6.4, chloride 103, CO2 (carbon dioxide) 16.8, BUN (blood urea nitrogen) and creatinine 92/8.7, glucose 74, and calcium 9. Hemogram shows H&H (hematocrit and hemoglobin) of 11.4/33.9.
Because of diarrhea, Clostridium difficile toxin was also studied, and this turned out to be negative.
ASSESSMENT/PLAN:
1. Chronic renal failure/end-stage renal disease (on maintenance hemodialysis Tuesday, Thursday, and Saturday for a total of ten sessions this month) secondary to the following:
A. Status post right-sided nephrectomy 7 years ago.
B. Left-sided renal artery stenosis/renal vascular hypertension.
C. Diabetes
2. The patient is tolerating dialysis without any problems. We will give her Zemplar 2.5 mcg (microgram) after dialysis.
T2-1A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): _______________________________________________
The patient is seen in the outpatient dialysis unit for the purpose of hemodialysis. Report only the monthly dialysis services of the physician for 4 or more visits during the month.
This 57-year-old patient is seen and examined during hemodialysis. Chart is reviewed. The patient appears to be hemodynamically stable and not in any form of respiratory distress or compromise. She is tolerating dialysis without any problems. Predialysis vital signs are stable. Blood pressure is 134/63, heart rate 57, and temperature 98.6 F. She weighs 139.8 pounds. Today, we will dialyze her using her left Perm-A-Cath for a total of 3 hours using an HP-150 dialyzer and a 2.0 potassium bath. We will give her a Heparin loading dose of 2000 units and then maintenance of 1 ml (milliliter) per hour.
At the present time, vital signs are stable. Blood pressure is 117/61, heart rate 57, and she is tolerating a blood flow rate of 350 mL per minute. Normocephalic and atraumatic. Pale palpebral conjunctivae. Anicteric sclerae. No nasal or aural discharge. Moist tongue and buccal mucosa. No pharyngeal hyperemia, congestion, or exudates. Supple neck. No lymphadenopathy; symmetrical chest. No retractions. Positive rhonchi. No crackles or wheezes. S1 (first heart sound) and S2 (second heart second) distinct. No S3 (third heart sound) or S4 (fourth heart sound). Regular rate and rhythm. Abdomen: Positive bowel sounds, soft and nontender. Status post below-knee amputation. Pulses are fair.
Latest labs performed 1 month ago are as follows: Sodium 136, potassium 6.4, chloride 103, CO2 (carbon dioxide) 16.8, BUN (blood urea nitrogen) and creatinine 92/8.7, glucose 74, and calcium 9. Hemogram shows H&H (hematocrit and hemoglobin) of 11.4/33.9.
Because of diarrhea, Clostridium difficile toxin was also studied, and this turned out to be negative.
ASSESSMENT/PLAN:
1. Chronic renal failure/end-stage renal disease (on maintenance hemodialysis Tuesday, Thursday, and Saturday for a total of ten sessions this month) secondary to the following:
A. Status post right-sided nephrectomy 7 years ago.
B. Left-sided renal artery stenosis/renal vascular hypertension.
C. Diabetes
2. The patient is tolerating dialysis without any problems. We will give her Zemplar 2.5 mcg (microgram) after dialysis.
T2-1A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): _______________________________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck


