Deck 1: Evaluation and Management Services
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/6
Play
Full screen (f)
Deck 1: Evaluation and Management Services
1
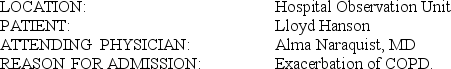
AUDIT REPORT T1.2 OBSERVATION
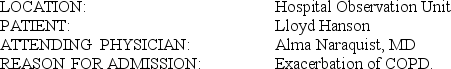 HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.
HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.
I proceeded by doing ABGs on him. His pH was 7.46, PCO2 94, bicarb 33.5 on 2 liters per nasal cannula.
The patient has some cough with clear phlegm. No fever or chills now. He had some chills a week ago.
The patient recently had an angiogram for his abdominal aortic aneurysm.He also had a stress test that apparently was positive.
The patient is known to have chronic renal failure with a baseline creatinine of 2 to 2.2 with creatinine clearance of 32 ml per minute with a serum creatinine of 2.0 back in December.
He does have severe congestive heart failure with ejection fraction less than 20%.
PAST MEDICAL HISTORY:
1. Chronic renal failure as mentioned.
2. Coronary artery disease, post two myocardial infarctions.
3. Post AICD placement.
4. Atrial fibrillation with rapid ventricular response, controlled.
5. Congestive heart failure with ejection fraction of less than 20%.
6. Abdominal aortic aneurysm, which is infrarenal measuring 6.2 cm.
7. Bilateral common iliac aneurysm, approximately 3.5 to 3.6 cm.
8. Left internal iliac artery aneurysm, questionably coiled lately.
9. COPD/asthma.
10. History of gouty arthritis with a recent gouty attack in his right first metatarsal phalangeal joint.
11. History of diverticulitis.
12. Hyperlipidemia.
13. Status post cholecystectomy, inguinal hernia repair, appendectomy.
14. Chronic renal failure, post PD catheter placement.
ALLERGIES: No known drug allergies.
MEDICATIONS:
1. Nebulizer at home.
2. Bumex 2 mg in the morning and 1 mg in the evening.
3. Coumadin 2 mg on Monday, 1 mg on other days.
4. Digoxin 0.125 mg po daily.
5. Potassium chloride 20 mEq po b.i.d.
6. Zocor 10 mg po q.hs.
7. Coreg 25 mg po b.i.d.
8. Allopurinol 100 mg po daily.
9. Ranitidine 150 mg po q.hs.
FAMILY HISTORY: Mother died of pancreatitis. Father died at age 71. Otherwise, family history is noncontributory.
SOCIAL HISTORY: Lives here in town with his wife. She was not available today. He quit smoking 16 years ago.
REVIEW OF SYSTEMS: CONSTITUTIONAL: No fever, chills, or night sweats.
ENT: Resolved upper-respiratory tract symptoms. RESPIRATORY: As mentioned.
CARDIOVASCULAR: Exertional dyspnea. No chest pain. GI: Questionable dark stool but no diarrhea, nausea, or vomiting. He had some abdominal discomfort with coughing. MUSCULOSKELETAL: History of gouty arthritis, but seems to be controlled. SKIN: Trace edema. NEURO: Negative. PSYCHIATRIC: Negative.
PHYSICAL EXAMINATION: The patient was in mild respiratory distress. He was awake, oriented times three without any focal neurological deficits. His heart rate is in the 70s range, blood pressure has been 120s/80s, sats 92% when he came in, 98% on 2 liters per nasal cannula. Slightly increased jugular venous pressure. No cervical lymphadenopathy. LUNGS: Good air entry bilaterally but expiratory wheezes bilaterally. No crackles. No sacral edema. ABDOMEN: Soft and nontender, no masses. He has PD catheter in the left lower quadrant. Small hematoma in the right inguinal area from his recent aortogram.
LOWER EXTREMITIES: Very trace edema.
LABORATORY STUDIES: CBC tonight shows a white count of 8.6 thousand, hemoglobin 12.3, platelets 140,000, BUN 29, sodium 139, potassium 3.6, chloride 98, bicarb 31, creatinine 2.2, calcium 8.5. BNP 536 picogram/ml. INR 1.5 with a pro-time of 14.3. Digoxin 0.6. Troponin-I less than 0.04. His last uric acid level was 7.4.
IMPRESSION:
1. Exacerbation of COPD/asthma with wheezes.
2. Abdominal aortic aneurysm.
PLAN:
1. Albuterol MDI 2 puffs t.i.d.
2. Atrovent MDI 2 puffs t.i.d.
3. Azmacort MDI 2 puffs b.i.d.
4. Solu-Medrol 80 mg IV q8h.
5. Continue the current PO medications.
6. Zithromax 500 mg IV daily.
7. The patient is code level I.
Discussed all of the above with the patient. He seems to understand and agrees with the plan.Will discuss further issues to his abdominal aortic aneurysm and further plans with his positive stress test when the rest of the family is available in the next couple of days.
T1.2:
SERVICE CODE(S): 99221____________________________________________
ICD-10-CM DX CODE(S): RO6.02, J44.1, I50.9___________________________
INCORRECT/MISSING CODE(S):_____________________________________
 HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.
HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.I proceeded by doing ABGs on him. His pH was 7.46, PCO2 94, bicarb 33.5 on 2 liters per nasal cannula.
The patient has some cough with clear phlegm. No fever or chills now. He had some chills a week ago.
The patient recently had an angiogram for his abdominal aortic aneurysm.He also had a stress test that apparently was positive.
The patient is known to have chronic renal failure with a baseline creatinine of 2 to 2.2 with creatinine clearance of 32 ml per minute with a serum creatinine of 2.0 back in December.
He does have severe congestive heart failure with ejection fraction less than 20%.
PAST MEDICAL HISTORY:
1. Chronic renal failure as mentioned.
2. Coronary artery disease, post two myocardial infarctions.
3. Post AICD placement.
4. Atrial fibrillation with rapid ventricular response, controlled.
5. Congestive heart failure with ejection fraction of less than 20%.
6. Abdominal aortic aneurysm, which is infrarenal measuring 6.2 cm.
7. Bilateral common iliac aneurysm, approximately 3.5 to 3.6 cm.
8. Left internal iliac artery aneurysm, questionably coiled lately.
9. COPD/asthma.
10. History of gouty arthritis with a recent gouty attack in his right first metatarsal phalangeal joint.
11. History of diverticulitis.
12. Hyperlipidemia.
13. Status post cholecystectomy, inguinal hernia repair, appendectomy.
14. Chronic renal failure, post PD catheter placement.
ALLERGIES: No known drug allergies.
MEDICATIONS:
1. Nebulizer at home.
2. Bumex 2 mg in the morning and 1 mg in the evening.
3. Coumadin 2 mg on Monday, 1 mg on other days.
4. Digoxin 0.125 mg po daily.
5. Potassium chloride 20 mEq po b.i.d.
6. Zocor 10 mg po q.hs.
7. Coreg 25 mg po b.i.d.
8. Allopurinol 100 mg po daily.
9. Ranitidine 150 mg po q.hs.
FAMILY HISTORY: Mother died of pancreatitis. Father died at age 71. Otherwise, family history is noncontributory.
SOCIAL HISTORY: Lives here in town with his wife. She was not available today. He quit smoking 16 years ago.
REVIEW OF SYSTEMS: CONSTITUTIONAL: No fever, chills, or night sweats.
ENT: Resolved upper-respiratory tract symptoms. RESPIRATORY: As mentioned.
CARDIOVASCULAR: Exertional dyspnea. No chest pain. GI: Questionable dark stool but no diarrhea, nausea, or vomiting. He had some abdominal discomfort with coughing. MUSCULOSKELETAL: History of gouty arthritis, but seems to be controlled. SKIN: Trace edema. NEURO: Negative. PSYCHIATRIC: Negative.
PHYSICAL EXAMINATION: The patient was in mild respiratory distress. He was awake, oriented times three without any focal neurological deficits. His heart rate is in the 70s range, blood pressure has been 120s/80s, sats 92% when he came in, 98% on 2 liters per nasal cannula. Slightly increased jugular venous pressure. No cervical lymphadenopathy. LUNGS: Good air entry bilaterally but expiratory wheezes bilaterally. No crackles. No sacral edema. ABDOMEN: Soft and nontender, no masses. He has PD catheter in the left lower quadrant. Small hematoma in the right inguinal area from his recent aortogram.
LOWER EXTREMITIES: Very trace edema.
LABORATORY STUDIES: CBC tonight shows a white count of 8.6 thousand, hemoglobin 12.3, platelets 140,000, BUN 29, sodium 139, potassium 3.6, chloride 98, bicarb 31, creatinine 2.2, calcium 8.5. BNP 536 picogram/ml. INR 1.5 with a pro-time of 14.3. Digoxin 0.6. Troponin-I less than 0.04. His last uric acid level was 7.4.
IMPRESSION:
1. Exacerbation of COPD/asthma with wheezes.
2. Abdominal aortic aneurysm.
PLAN:
1. Albuterol MDI 2 puffs t.i.d.
2. Atrovent MDI 2 puffs t.i.d.
3. Azmacort MDI 2 puffs b.i.d.
4. Solu-Medrol 80 mg IV q8h.
5. Continue the current PO medications.
6. Zithromax 500 mg IV daily.
7. The patient is code level I.
Discussed all of the above with the patient. He seems to understand and agrees with the plan.Will discuss further issues to his abdominal aortic aneurysm and further plans with his positive stress test when the rest of the family is available in the next couple of days.
T1.2:
SERVICE CODE(S): 99221____________________________________________
ICD-10-CM DX CODE(S): RO6.02, J44.1, I50.9___________________________
INCORRECT/MISSING CODE(S):_____________________________________
INCORRECT/MISSING CODE(S): 99218, R06.02, I71.4
2
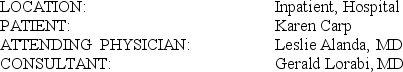
T1-2B CONSULTATION
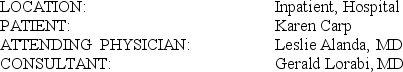 REASON FOR CONSULTATION: Dr. Alanda asked me to see the patient over concerns that she might have an autoimmune hemolytic anemia.
REASON FOR CONSULTATION: Dr. Alanda asked me to see the patient over concerns that she might have an autoimmune hemolytic anemia.
HISTORY: The patient is a 59-year-old female who has had a stormy course after open reduction internal fixation of a supracondylar fracture of her left femur. Postoperatively, she developed respiratory problems, ARDS (acute or adult respiratory distress syndrome), and also has been felt to have a cholestatic liver problem.
Chief problem is that her bilirubin is over 4. Her hemoglobin has failed below 7 g, and she has increased reticulocytes. She has been transfused recently several units and despite that her hemoglobin has dropped. Dr. Alanda was under the impression that her direct Coombs' test was positive but in checking into this further, her direct antiglobulin test was negative, but she did have multiple other alloantibodies.
In reviewing the chart, her past history is significant for coronary artery disease, obesity, hypertension, tobacco abuse, and hyperlipidemia. She had a right CVA (stroke/cardiovascular accident) with hemiparesis last year.
From the chart, I am not aware if she previously had blood transfusion.
MEDICATIONS: She is on a panoply of medications as listed in Dr. Naraquist's consultation notes.
ALLERGIES: None known.
SOCIAL HISTORY: No significant alcohol abuse, but a 2-pack-a-day smoker. She does not work outside the home.
FAMILY HISTORY: Her mother died of leukemia. Father died of congestive heart failure at age 58. A sister died at age 29 of a myocardial infarction.
REVIEW OF SYSTEMS: At this time is impossible as the patient is sedated on a ventilator and unresponsive to questions.
She has hepatitis serology and HIV (human immunodeficiency virus) serology pending at the time of this dictation. Clotting studies were negative. Her Coombs' test was negative as mentioned above and antibody screen was positive. Reticulocytes were done late last night and absolute reticulocyte count was 113,000. Recent troponin level was negative.
PHYSICAL EXAMINATION: The patient is moribund. She is obese. She is sedated at this time on a ventilator. Vital signs are being maintained within a reasonable range at this point. She is not grossly jaundiced. Lungs reveal diminished air entry. Heart tones are normal and regular. Her abdomen is massively obese. No definite liver or splenic enlargement. No external bruising noted. Sclerae may be slightly icteric. No lymphadenopathy. There is no gross edema appreciated in extremities. She has a Foley catheter in place and the urine from that is pink. Other formal testing was not possible because of the patient's condition.
I spent time looking at her peripheral smear. She does have enucleated red cells in the peripheral smear and a left shift. This is probably a leukoerythroblastic reaction related to some hemolysis and to her recent ARDS and surgical procedure. There are no increased numbers of spherocytes noted. There is significant polychromasia. Her liver functions were significantly abnormal with elevation of her hepatic enzymes and her bilirubin was as high as 9.6, but is down to 4. Almost all this bilirubin is direct reacting which would certainly be more consistent with hepatic disease on the face of hemolysis or excessive bleeding.
IMPRESSION:
1. Significant anemia, which probably is related to hemolysis. This, at least in part, is probably related to alloantibodies and engendered by her recent blood transfusion. She had no antibodies, probably a result of the transfusion and probably a result of previous exposure to blood transfusion. The elevated bilirubin is in part due to her hemolysis and in part due to impaired hepatic function. There is no evidence of autoimmune hemolytic anemia in her case.
2. ARDS (acute or adult respiratory distress syndrome).
3. Obesity.
In this situation, it would be critical to give plenty of IV (intravenous) fluids with appropriate diuresis to try and maintain adequate urine flow.
Thank you for this consultation.
T1-2B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
 REASON FOR CONSULTATION: Dr. Alanda asked me to see the patient over concerns that she might have an autoimmune hemolytic anemia.
REASON FOR CONSULTATION: Dr. Alanda asked me to see the patient over concerns that she might have an autoimmune hemolytic anemia.HISTORY: The patient is a 59-year-old female who has had a stormy course after open reduction internal fixation of a supracondylar fracture of her left femur. Postoperatively, she developed respiratory problems, ARDS (acute or adult respiratory distress syndrome), and also has been felt to have a cholestatic liver problem.
Chief problem is that her bilirubin is over 4. Her hemoglobin has failed below 7 g, and she has increased reticulocytes. She has been transfused recently several units and despite that her hemoglobin has dropped. Dr. Alanda was under the impression that her direct Coombs' test was positive but in checking into this further, her direct antiglobulin test was negative, but she did have multiple other alloantibodies.
In reviewing the chart, her past history is significant for coronary artery disease, obesity, hypertension, tobacco abuse, and hyperlipidemia. She had a right CVA (stroke/cardiovascular accident) with hemiparesis last year.
From the chart, I am not aware if she previously had blood transfusion.
MEDICATIONS: She is on a panoply of medications as listed in Dr. Naraquist's consultation notes.
ALLERGIES: None known.
SOCIAL HISTORY: No significant alcohol abuse, but a 2-pack-a-day smoker. She does not work outside the home.
FAMILY HISTORY: Her mother died of leukemia. Father died of congestive heart failure at age 58. A sister died at age 29 of a myocardial infarction.
REVIEW OF SYSTEMS: At this time is impossible as the patient is sedated on a ventilator and unresponsive to questions.
She has hepatitis serology and HIV (human immunodeficiency virus) serology pending at the time of this dictation. Clotting studies were negative. Her Coombs' test was negative as mentioned above and antibody screen was positive. Reticulocytes were done late last night and absolute reticulocyte count was 113,000. Recent troponin level was negative.
PHYSICAL EXAMINATION: The patient is moribund. She is obese. She is sedated at this time on a ventilator. Vital signs are being maintained within a reasonable range at this point. She is not grossly jaundiced. Lungs reveal diminished air entry. Heart tones are normal and regular. Her abdomen is massively obese. No definite liver or splenic enlargement. No external bruising noted. Sclerae may be slightly icteric. No lymphadenopathy. There is no gross edema appreciated in extremities. She has a Foley catheter in place and the urine from that is pink. Other formal testing was not possible because of the patient's condition.
I spent time looking at her peripheral smear. She does have enucleated red cells in the peripheral smear and a left shift. This is probably a leukoerythroblastic reaction related to some hemolysis and to her recent ARDS and surgical procedure. There are no increased numbers of spherocytes noted. There is significant polychromasia. Her liver functions were significantly abnormal with elevation of her hepatic enzymes and her bilirubin was as high as 9.6, but is down to 4. Almost all this bilirubin is direct reacting which would certainly be more consistent with hepatic disease on the face of hemolysis or excessive bleeding.
IMPRESSION:
1. Significant anemia, which probably is related to hemolysis. This, at least in part, is probably related to alloantibodies and engendered by her recent blood transfusion. She had no antibodies, probably a result of the transfusion and probably a result of previous exposure to blood transfusion. The elevated bilirubin is in part due to her hemolysis and in part due to impaired hepatic function. There is no evidence of autoimmune hemolytic anemia in her case.
2. ARDS (acute or adult respiratory distress syndrome).
3. Obesity.
In this situation, it would be critical to give plenty of IV (intravenous) fluids with appropriate diuresis to try and maintain adequate urine flow.
Thank you for this consultation.
T1-2B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Professional Services: 99255 (Evaluation and Management, Consultation)
ICD-10-CM DX: D64.9 (Anemia), K72.90 (Impaired/impairment, liver), J80 (Syndrome, respiratory distress, acute, adult), E66.9 (Obesity), Z99.11 (Dependence, on, ventilator)
ICD-10-CM DX: D64.9 (Anemia), K72.90 (Impaired/impairment, liver), J80 (Syndrome, respiratory distress, acute, adult), E66.9 (Obesity), Z99.11 (Dependence, on, ventilator)
3
T1-1B CRITICAL CARE SERVICE
Dr. Sutton, emergency room physician, called in Dr. Elhart, the cardiologist on call from the local clinic, to provide critical care services to Linda Paulo. Code the services provided by Dr. Elhart in the following case.
The patient is a 23-year-old Hispanic female who took some medications to sleep tonight, including what sounds like amitriptyline and Hydrocodone. She called her husband, who came over at approximately 9:30 tonight. She slept for an hour until 10:30, and then she started having generalized seizures on and off four times, during which her husband called 911. Paramedics were on the scene in 4 to 5 minutes. The patient was immediately intubated. Monitor showed wide QRS (Q-wave, R-wave, S-wave) complexes. She received bicarbonate and was sent to the emergency room. I saw her with Dr. Sutton in the emergency room. She was actively seizing. She received multiple doses of Ativan, and then I gave her around 20 mg (milligram) of Versed and started a Versed drip. She was on a bicarbonate drip, and we gave her multiple amps of bicarbonate. Her QRS narrowed down. Unfortunately, this did not last long. The patient went bradycardic and then went into a junctional rhythm. Her blood pressure was dropping on occasion and then coming back up again. She eventually coded. We resuscitated her for more than 20 minutes. She had multiple rhythm problems including asystole, ventricular tachycardia, and pulseless electrical activity. She received multiple doses of epinephrine and multiple amps of sodium bicarbonate. She eventually recovered back in sinus rhythm after defibrillation for ventricular tachycardia.
Her ABGs (arterial blood gases) initially were pH (potential of hydrogen) 74.8 and PCO2 (partial pressure of carbon dioxide) 28. Oxygen was around 500 on 100% FiO2 (forced inspiration oxygen) with a bicarb of 18. Her bicarb went up to 23 at the end of the code when she was in sinus rhythm. She was transferred up to the floor with three IVs (intravenous) running at 999.
On the floor, her blood pressure dropped again to 50. She went bradycardic and coded. She received at least two shocks. She received again multiple doses of epinephrine and received multiple sodium bicarbonate amps, at least eight.
Discussions were held with the husband multiple times since admission with Dr. Sutton and myself. I brought him to the room while the patient was getting CPR (cardiopulmonary resuscitation) the second time. After 20 minutes, the patient was having no cardiac activity whatsoever, and after 20 minutes decided to stop CPR after discussing this with her husband.
DISCHARGE DIAGNOSIS: Cardiac arrest, tricyclic antidepressant, resulting in severe neural and cardiac toxicity and eventually resulting in death.
Time spent with patient was 120 minutes.
T1-1B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Dr. Sutton, emergency room physician, called in Dr. Elhart, the cardiologist on call from the local clinic, to provide critical care services to Linda Paulo. Code the services provided by Dr. Elhart in the following case.
The patient is a 23-year-old Hispanic female who took some medications to sleep tonight, including what sounds like amitriptyline and Hydrocodone. She called her husband, who came over at approximately 9:30 tonight. She slept for an hour until 10:30, and then she started having generalized seizures on and off four times, during which her husband called 911. Paramedics were on the scene in 4 to 5 minutes. The patient was immediately intubated. Monitor showed wide QRS (Q-wave, R-wave, S-wave) complexes. She received bicarbonate and was sent to the emergency room. I saw her with Dr. Sutton in the emergency room. She was actively seizing. She received multiple doses of Ativan, and then I gave her around 20 mg (milligram) of Versed and started a Versed drip. She was on a bicarbonate drip, and we gave her multiple amps of bicarbonate. Her QRS narrowed down. Unfortunately, this did not last long. The patient went bradycardic and then went into a junctional rhythm. Her blood pressure was dropping on occasion and then coming back up again. She eventually coded. We resuscitated her for more than 20 minutes. She had multiple rhythm problems including asystole, ventricular tachycardia, and pulseless electrical activity. She received multiple doses of epinephrine and multiple amps of sodium bicarbonate. She eventually recovered back in sinus rhythm after defibrillation for ventricular tachycardia.
Her ABGs (arterial blood gases) initially were pH (potential of hydrogen) 74.8 and PCO2 (partial pressure of carbon dioxide) 28. Oxygen was around 500 on 100% FiO2 (forced inspiration oxygen) with a bicarb of 18. Her bicarb went up to 23 at the end of the code when she was in sinus rhythm. She was transferred up to the floor with three IVs (intravenous) running at 999.
On the floor, her blood pressure dropped again to 50. She went bradycardic and coded. She received at least two shocks. She received again multiple doses of epinephrine and received multiple sodium bicarbonate amps, at least eight.
Discussions were held with the husband multiple times since admission with Dr. Sutton and myself. I brought him to the room while the patient was getting CPR (cardiopulmonary resuscitation) the second time. After 20 minutes, the patient was having no cardiac activity whatsoever, and after 20 minutes decided to stop CPR after discussing this with her husband.
DISCHARGE DIAGNOSIS: Cardiac arrest, tricyclic antidepressant, resulting in severe neural and cardiac toxicity and eventually resulting in death.
Time spent with patient was 120 minutes.
T1-1B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Professional Services: 99291 (Evaluation and Management, Critical Care), 99292 2 (Evaluation and Management, Critical Care)
ICD-10-CM DX: T43.021A (Table of Drugs and Chemicals, Amitriptyline), T40.2X1A (Table of Drugs and Chemicals, Hydrocodone), I46.9 (Arrest/arrested, cardiac)
ICD-10-CM DX: T43.021A (Table of Drugs and Chemicals, Amitriptyline), T40.2X1A (Table of Drugs and Chemicals, Hydrocodone), I46.9 (Arrest/arrested, cardiac)
4
T1-2A INITIAL HOSPITAL CARE
 HISTORY: This lady is a 34-year-old married white female, gravida 2, para (to bring forth) 2. Her LMP (last menstrual period) was April 30, and she received an injection of Depo-Provera at 200 mg (milligram) IM (intramuscular) on May 2. The patient has a long-standing history of endometriosis dating back to June 10 years ago when she had bilateral ovarian cystectomies for endometriosis in her hometown. She was then treated with Danazol for 6 months. I saw her initially back 3 years ago for secondary infertility. She had a laparoscopy with lysis of adhesions the following year, at which time the right ovary was mildly adherent to the pelvic sidewall but was broken up somewhat with dissection, and she had some small bowel adherent to the left ovary. She was then treated on multiple cycles of Klonopin citrate because of luteal phase deficiency but failed to conceive. Last year, she underwent repeat laparoscopy with exploratory laparotomy and pelvic adhesiolysis, having had bowel and pelvic adhesions, and she had resection of several areas of endometriosis. At that point, the patient continued to try and get pregnant but was having more problems; therefore, she was treated with oral contraceptives and nonsteroidal anti-inflammatory drugs. The patient did spontaneously conceive and delivered her second child on August 20. She was not having much success in alleviating her symptoms of dysmenorrhea and dyspareunia; therefore, she was begun on continuous oral contraceptives in the form of Demulen 1/50 back in January. This did result in the expected amenorrhea, and her symptoms were initially controlled fairly well. She then started having more in the way of cramping and pain; however, dyspareunia had improved. At this point, she is being brought in for definitive surgery because of persistent pelvic pain and cramping.
HISTORY: This lady is a 34-year-old married white female, gravida 2, para (to bring forth) 2. Her LMP (last menstrual period) was April 30, and she received an injection of Depo-Provera at 200 mg (milligram) IM (intramuscular) on May 2. The patient has a long-standing history of endometriosis dating back to June 10 years ago when she had bilateral ovarian cystectomies for endometriosis in her hometown. She was then treated with Danazol for 6 months. I saw her initially back 3 years ago for secondary infertility. She had a laparoscopy with lysis of adhesions the following year, at which time the right ovary was mildly adherent to the pelvic sidewall but was broken up somewhat with dissection, and she had some small bowel adherent to the left ovary. She was then treated on multiple cycles of Klonopin citrate because of luteal phase deficiency but failed to conceive. Last year, she underwent repeat laparoscopy with exploratory laparotomy and pelvic adhesiolysis, having had bowel and pelvic adhesions, and she had resection of several areas of endometriosis. At that point, the patient continued to try and get pregnant but was having more problems; therefore, she was treated with oral contraceptives and nonsteroidal anti-inflammatory drugs. The patient did spontaneously conceive and delivered her second child on August 20. She was not having much success in alleviating her symptoms of dysmenorrhea and dyspareunia; therefore, she was begun on continuous oral contraceptives in the form of Demulen 1/50 back in January. This did result in the expected amenorrhea, and her symptoms were initially controlled fairly well. She then started having more in the way of cramping and pain; however, dyspareunia had improved. At this point, she is being brought in for definitive surgery because of persistent pelvic pain and cramping.
CURRENT MEDICATIONS: None
ALLERGIES: None
REVIEW OF SYSTEMS: She has occasional lower abdominal cramping, but this has improved somewhat since her injection of Depo-Provera. She has no URI (upper respiratory infection) symptoms or cough. No GI (gastrointestinal) or GU (genitourinary) symptoms. No vaginal discharge.
FAMILY HISTORY: Her dad has maturity onset diabetes, coronary artery disease, and hypertension, but he is living. Her mom is in good health. She had two maternal aunts with breast cancer, and there are other types of cancer in her mother's siblings, the specifics of which are unknown.
SOCIAL HISTORY: The patient is a teacher at the local elementary school in her hometown. Habits: Occasional alcohol. Very rarely does she smoke a cigarette.
PAST SURGICAL HISTORY:
1. Laparoscopy, exploratory laparotomy with adhesiolysis.
2. Ovarian cystectomy and appendectomy.
3. Diagnostic laparoscopy.
PHYSICAL EXAMINATION: Weight is 162 pounds. Blood pressure is 100/60. Pulse, 60. HEENT (head, ears, eyes, nose, throat) are unremarkable. Neck has no masses. Lungs are clear to auscultation. Heart has a regular rhythm without audible murmurs or gallops. Breasts are negative. Abdomen is soft and shows a laparoscopy scar and Pfannenstiel scar. Vulva and vagina are normal. Cervix is parous. Uterus is anterior and normal size. Adnexa reveal tenderness on the left but not on the right. On rectovaginal examination, there is some extreme nodularity on the left side of the cul-de-sac. Extremities show no phlebitis.
LABORATORY STUDIES: Preop laboratory work shows the urinalysis to be normal. White count is 5440. Hemoglobin is 13.6 g (gram).
PREOPERATIVE DIAGNOSIS: Endometriosis with chronic dysmenorrhea and pelvic pain.
OPERATIVE PLAN: Total abdominal hysterectomy and bilateral salpingo-oophorectomy. The patient will receive a mechanical and antibiotic bowel prep, and she will also have ureteral catheters placed preoperatively by Dr. Avila. The patient understands the potential complications, infections, bleeding, bowel, bladder, and ureteral injury. Potential complications of blood clot formation and pulmonary emboli are also discussed with the patient. She understands the necessity of the operation, its intended outcome and risks, and agrees to proceed as planned.
T1-2A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
 HISTORY: This lady is a 34-year-old married white female, gravida 2, para (to bring forth) 2. Her LMP (last menstrual period) was April 30, and she received an injection of Depo-Provera at 200 mg (milligram) IM (intramuscular) on May 2. The patient has a long-standing history of endometriosis dating back to June 10 years ago when she had bilateral ovarian cystectomies for endometriosis in her hometown. She was then treated with Danazol for 6 months. I saw her initially back 3 years ago for secondary infertility. She had a laparoscopy with lysis of adhesions the following year, at which time the right ovary was mildly adherent to the pelvic sidewall but was broken up somewhat with dissection, and she had some small bowel adherent to the left ovary. She was then treated on multiple cycles of Klonopin citrate because of luteal phase deficiency but failed to conceive. Last year, she underwent repeat laparoscopy with exploratory laparotomy and pelvic adhesiolysis, having had bowel and pelvic adhesions, and she had resection of several areas of endometriosis. At that point, the patient continued to try and get pregnant but was having more problems; therefore, she was treated with oral contraceptives and nonsteroidal anti-inflammatory drugs. The patient did spontaneously conceive and delivered her second child on August 20. She was not having much success in alleviating her symptoms of dysmenorrhea and dyspareunia; therefore, she was begun on continuous oral contraceptives in the form of Demulen 1/50 back in January. This did result in the expected amenorrhea, and her symptoms were initially controlled fairly well. She then started having more in the way of cramping and pain; however, dyspareunia had improved. At this point, she is being brought in for definitive surgery because of persistent pelvic pain and cramping.
HISTORY: This lady is a 34-year-old married white female, gravida 2, para (to bring forth) 2. Her LMP (last menstrual period) was April 30, and she received an injection of Depo-Provera at 200 mg (milligram) IM (intramuscular) on May 2. The patient has a long-standing history of endometriosis dating back to June 10 years ago when she had bilateral ovarian cystectomies for endometriosis in her hometown. She was then treated with Danazol for 6 months. I saw her initially back 3 years ago for secondary infertility. She had a laparoscopy with lysis of adhesions the following year, at which time the right ovary was mildly adherent to the pelvic sidewall but was broken up somewhat with dissection, and she had some small bowel adherent to the left ovary. She was then treated on multiple cycles of Klonopin citrate because of luteal phase deficiency but failed to conceive. Last year, she underwent repeat laparoscopy with exploratory laparotomy and pelvic adhesiolysis, having had bowel and pelvic adhesions, and she had resection of several areas of endometriosis. At that point, the patient continued to try and get pregnant but was having more problems; therefore, she was treated with oral contraceptives and nonsteroidal anti-inflammatory drugs. The patient did spontaneously conceive and delivered her second child on August 20. She was not having much success in alleviating her symptoms of dysmenorrhea and dyspareunia; therefore, she was begun on continuous oral contraceptives in the form of Demulen 1/50 back in January. This did result in the expected amenorrhea, and her symptoms were initially controlled fairly well. She then started having more in the way of cramping and pain; however, dyspareunia had improved. At this point, she is being brought in for definitive surgery because of persistent pelvic pain and cramping.CURRENT MEDICATIONS: None
ALLERGIES: None
REVIEW OF SYSTEMS: She has occasional lower abdominal cramping, but this has improved somewhat since her injection of Depo-Provera. She has no URI (upper respiratory infection) symptoms or cough. No GI (gastrointestinal) or GU (genitourinary) symptoms. No vaginal discharge.
FAMILY HISTORY: Her dad has maturity onset diabetes, coronary artery disease, and hypertension, but he is living. Her mom is in good health. She had two maternal aunts with breast cancer, and there are other types of cancer in her mother's siblings, the specifics of which are unknown.
SOCIAL HISTORY: The patient is a teacher at the local elementary school in her hometown. Habits: Occasional alcohol. Very rarely does she smoke a cigarette.
PAST SURGICAL HISTORY:
1. Laparoscopy, exploratory laparotomy with adhesiolysis.
2. Ovarian cystectomy and appendectomy.
3. Diagnostic laparoscopy.
PHYSICAL EXAMINATION: Weight is 162 pounds. Blood pressure is 100/60. Pulse, 60. HEENT (head, ears, eyes, nose, throat) are unremarkable. Neck has no masses. Lungs are clear to auscultation. Heart has a regular rhythm without audible murmurs or gallops. Breasts are negative. Abdomen is soft and shows a laparoscopy scar and Pfannenstiel scar. Vulva and vagina are normal. Cervix is parous. Uterus is anterior and normal size. Adnexa reveal tenderness on the left but not on the right. On rectovaginal examination, there is some extreme nodularity on the left side of the cul-de-sac. Extremities show no phlebitis.
LABORATORY STUDIES: Preop laboratory work shows the urinalysis to be normal. White count is 5440. Hemoglobin is 13.6 g (gram).
PREOPERATIVE DIAGNOSIS: Endometriosis with chronic dysmenorrhea and pelvic pain.
OPERATIVE PLAN: Total abdominal hysterectomy and bilateral salpingo-oophorectomy. The patient will receive a mechanical and antibiotic bowel prep, and she will also have ureteral catheters placed preoperatively by Dr. Avila. The patient understands the potential complications, infections, bleeding, bowel, bladder, and ureteral injury. Potential complications of blood clot formation and pulmonary emboli are also discussed with the patient. She understands the necessity of the operation, its intended outcome and risks, and agrees to proceed as planned.
T1-2A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
5
T1-1A EMERGENCY AND OUTPATIENT RECORD
 This is a 17-year-old male who comes in after he got punched in the right side of his face. Mother is concerned because he is a diabetic and has a couple of lip lacerations, also complained of some transient blurry vision, which has since improved. The patient states that he did get hit on the right cheek area. Immediately following this he had some blurry vision in the right eye, which slowly has improved and is near normal now. He also notes that he had a cut on his right lower lip and upper inside of his right lip as well. No other complaints. Visual acuity is 20/40 both. Note the patient normally wears glasses but did not have them for this examination.
This is a 17-year-old male who comes in after he got punched in the right side of his face. Mother is concerned because he is a diabetic and has a couple of lip lacerations, also complained of some transient blurry vision, which has since improved. The patient states that he did get hit on the right cheek area. Immediately following this he had some blurry vision in the right eye, which slowly has improved and is near normal now. He also notes that he had a cut on his right lower lip and upper inside of his right lip as well. No other complaints. Visual acuity is 20/40 both. Note the patient normally wears glasses but did not have them for this examination.
PHYSICAL EXAMINATION: Head is normocephalic. PERRLA (pupils equal, round, reactive to light and accommodation). EOMS (extraocular movements) intact. Funduscopic examination is normal. There are no hemorrhages. Good sharp discs bilaterally. The discs appear clear bilaterally. TMs (tympanic membranes) are normal. Nose is without discharge. He has some tenderness and erythema in the right cheek where he was hit, no obvious swelling. Right upper lip: He had a 1- to 1.5-cm (centimeter) laceration. Superficial skin edges are not opposed, not bleeding. The teeth are in good repair. The right lower lip above the vermilion border has an abrasion. He opens and closes the jaw well. No TMJ (temporomandibular joint) tenderness. Neck is soft and supple.
ASSESSMENT:
1. Upper inner lip laceration, requiring simple suture repair.
2. Lower lip abrasion.
3. Right cheek contusion.
PLAN: Discussed my findings and diagnoses with the mother. I reassured her that the laceration was minor and only required two sutures to close adequately. She was advised to keep the area clean and to make an appointment with the family practitioner for removal of sutures in 7 days. He may rinse with some hydrogen peroxide and water. Watch for signs of infection; follow up if any occur. Continue to check blood sugars as stress can sometimes make these go off. Use some ice on the lip and right cheek. Follow up if any problems.
T1-1A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
 This is a 17-year-old male who comes in after he got punched in the right side of his face. Mother is concerned because he is a diabetic and has a couple of lip lacerations, also complained of some transient blurry vision, which has since improved. The patient states that he did get hit on the right cheek area. Immediately following this he had some blurry vision in the right eye, which slowly has improved and is near normal now. He also notes that he had a cut on his right lower lip and upper inside of his right lip as well. No other complaints. Visual acuity is 20/40 both. Note the patient normally wears glasses but did not have them for this examination.
This is a 17-year-old male who comes in after he got punched in the right side of his face. Mother is concerned because he is a diabetic and has a couple of lip lacerations, also complained of some transient blurry vision, which has since improved. The patient states that he did get hit on the right cheek area. Immediately following this he had some blurry vision in the right eye, which slowly has improved and is near normal now. He also notes that he had a cut on his right lower lip and upper inside of his right lip as well. No other complaints. Visual acuity is 20/40 both. Note the patient normally wears glasses but did not have them for this examination.PHYSICAL EXAMINATION: Head is normocephalic. PERRLA (pupils equal, round, reactive to light and accommodation). EOMS (extraocular movements) intact. Funduscopic examination is normal. There are no hemorrhages. Good sharp discs bilaterally. The discs appear clear bilaterally. TMs (tympanic membranes) are normal. Nose is without discharge. He has some tenderness and erythema in the right cheek where he was hit, no obvious swelling. Right upper lip: He had a 1- to 1.5-cm (centimeter) laceration. Superficial skin edges are not opposed, not bleeding. The teeth are in good repair. The right lower lip above the vermilion border has an abrasion. He opens and closes the jaw well. No TMJ (temporomandibular joint) tenderness. Neck is soft and supple.
ASSESSMENT:
1. Upper inner lip laceration, requiring simple suture repair.
2. Lower lip abrasion.
3. Right cheek contusion.
PLAN: Discussed my findings and diagnoses with the mother. I reassured her that the laceration was minor and only required two sutures to close adequately. She was advised to keep the area clean and to make an appointment with the family practitioner for removal of sutures in 7 days. He may rinse with some hydrogen peroxide and water. Watch for signs of infection; follow up if any occur. Continue to check blood sugars as stress can sometimes make these go off. Use some ice on the lip and right cheek. Follow up if any problems.
T1-1A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck
6
AUDIT REPORT T1.1 OFFICE VISIT
 He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.
He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.
His DM has been variably controlled. He is taking Lantus 28 units in the evening and Humalog 12 units with meals. He is testing 2-4 times per day. He is having reactions around 3 PM about once a week. He does get a warning with the reactions. His sugars are highly variable at all testing times with high and low sugars. His evening sugars tend to be high, and he may overeat after supper.
He continues to have numbness in the feet. There is no edema. His depression seems to be ok.
EXAM: Vitals:Weight is 180. Blood pressure is 120/70. Patient is alert and conversant.
He is near his ideal weight. There is no edema. The foot pulses are normal. The ankle and knee reflexes are normal. There is a slight decrease in the vibratory sensation. The chest is clear. Cardiac: The heart is regular with no murmur or S3. The abdomen is soft and nontender with no masses. The prostate is a little enlarged with no masses. The rectum is normal, and there are some small hemorrhoids noted. The stool is hemoccult negative.
IMPRESSION: 1) DM Type 1 with variable control, 2) Hemorrhoids, 3) CAD, stable.
PLAN: Anusol suppository bid prn and tub soaks. He may need to cut the noon Humalog by 2 units. See in 4 months with an HgbA1c.
T1.1:
SERVICE CODE(S): 99213_________________________________
ICD-10-CM DX CODE(S): E10.9____________________________
INCORRECT/MISSING CODE(S):__________________________
 He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.
He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.His DM has been variably controlled. He is taking Lantus 28 units in the evening and Humalog 12 units with meals. He is testing 2-4 times per day. He is having reactions around 3 PM about once a week. He does get a warning with the reactions. His sugars are highly variable at all testing times with high and low sugars. His evening sugars tend to be high, and he may overeat after supper.
He continues to have numbness in the feet. There is no edema. His depression seems to be ok.
EXAM: Vitals:Weight is 180. Blood pressure is 120/70. Patient is alert and conversant.
He is near his ideal weight. There is no edema. The foot pulses are normal. The ankle and knee reflexes are normal. There is a slight decrease in the vibratory sensation. The chest is clear. Cardiac: The heart is regular with no murmur or S3. The abdomen is soft and nontender with no masses. The prostate is a little enlarged with no masses. The rectum is normal, and there are some small hemorrhoids noted. The stool is hemoccult negative.
IMPRESSION: 1) DM Type 1 with variable control, 2) Hemorrhoids, 3) CAD, stable.
PLAN: Anusol suppository bid prn and tub soaks. He may need to cut the noon Humalog by 2 units. See in 4 months with an HgbA1c.
T1.1:
SERVICE CODE(S): 99213_________________________________
ICD-10-CM DX CODE(S): E10.9____________________________
INCORRECT/MISSING CODE(S):__________________________

Unlock Deck
Unlock for access to all 6 flashcards in this deck.
Unlock Deck
k this deck


