Deck 11: Integrated Dynamics of Innate and Adaptive Immunity
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/28
Play
Full screen (f)
Deck 11: Integrated Dynamics of Innate and Adaptive Immunity
1
Nitric oxide and superoxide radicals are toxic compounds that induce substantial DNA damage. When released by activated M1 macrophages, these compounds cause damage to microbial pathogens and may also cause damage to host cells in the vicinity.
True
2
A set of mice are each immunized with one of the following as shown in Figure. 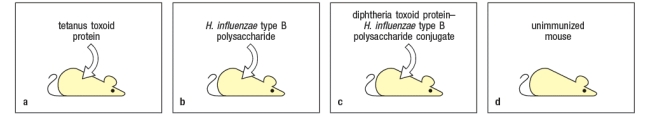
Mouse A is immunized with tetanus toxoid protein. Mouse B is immunized with the Haemophilus influenzae type b polysaccharide antigen. Mouse C is immunized with a conjugate of the diphtheria toxoid protein linked to H. influenzae type b polysaccharide. Mouse D is left unimmunized (naive). Four weeks later the spleen cells from each mouse are isolated, and B lymphocytes and T lymphocytes from each spleen cell population are purified. When mixed together in culture together with a conjugate antigen of the tetanus toxoid protein linked to the to H. influenzae type b polysaccharide, which combination of spleen cells would generate a memory B cell response?
A) B lymphocytes from mouse B plus T lymphocytes from mouse B
B) B lymphocytes from mouse A plus T lymphocytes from mouse A
C) B lymphocytes from mouse C plus T lymphocytes from mouse A
D) B lymphocytes from mouse C plus T lymphocytes from mouse D
E) B lymphocytes from mouse B plus T lymphocytes from mouse D
Mouse A is immunized with tetanus toxoid protein. Mouse B is immunized with the Haemophilus influenzae type b polysaccharide antigen. Mouse C is immunized with a conjugate of the diphtheria toxoid protein linked to H. influenzae type b polysaccharide. Mouse D is left unimmunized (naive). Four weeks later the spleen cells from each mouse are isolated, and B lymphocytes and T lymphocytes from each spleen cell population are purified. When mixed together in culture together with a conjugate antigen of the tetanus toxoid protein linked to the to H. influenzae type b polysaccharide, which combination of spleen cells would generate a memory B cell response?
A) B lymphocytes from mouse B plus T lymphocytes from mouse B
B) B lymphocytes from mouse A plus T lymphocytes from mouse A
C) B lymphocytes from mouse C plus T lymphocytes from mouse A
D) B lymphocytes from mouse C plus T lymphocytes from mouse D
E) B lymphocytes from mouse B plus T lymphocytes from mouse D
B lymphocytes from mouse C plus T lymphocytes from mouse A
3
Initially after an infection, the majority of the T cells present in the tissue at a site of infection are not specific for the infecting pathogen, but over the course of several days, this changes and antigen-specific T cells become enriched at this site. This is because:
A) T cells do not use their T-cell receptors during extravasation from blood into tissues.
B) Early after infection, there are few antigen-specific T cells in the host.
C) Naive T cells do not express the homing receptors to extravasate into sites of inflammation.
D) T cells up-regulate CD69 early after activation and are retained in the lymphoid organs.
E) T cells require several days to down-regulate CCR7.
A) T cells do not use their T-cell receptors during extravasation from blood into tissues.
B) Early after infection, there are few antigen-specific T cells in the host.
C) Naive T cells do not express the homing receptors to extravasate into sites of inflammation.
D) T cells up-regulate CD69 early after activation and are retained in the lymphoid organs.
E) T cells require several days to down-regulate CCR7.
T cells do not use their T-cell receptors during extravasation from blood into tissues.
4
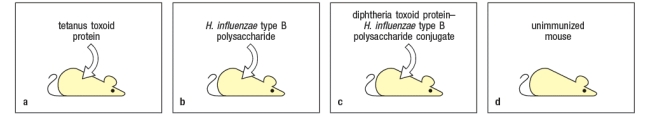
Toxoplasma gondii is a single-celled parasitic protozoan that infects and replicates in macrophages. It is common in the environment, and is transmitted to humans by the ingestion of undercooked meat or by accidental ingestion of the parasite's oocytes from contaminated water or cat litter. Infected individuals with healthy immune systems are generally asymptomatic, and rapidly clear the infection. However, in AIDS patients, infections of Toxoplasma gondii can lead to severe disease and even death. To investigate the immune mechanisms important in controlling Toxoplasma gondii, a mouse model of the infection was developed. Mice were infected with the protozoa at a dose where the majority of the mice survive the infection, and at the same time, were injected with a neutralizing antibody to a cytokine made by T cells (anti-'X' IgG). A second group of mice received the protozoa plus a control IgG antibody, as shown in Figure Q10). 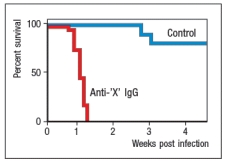 Figure Q10) The most likely candidate for cytokine 'X' is:
Figure Q10) The most likely candidate for cytokine 'X' is:
A) IFN-
B) IL-2
C) IL-4
D) IL-17
E) GM-CSF
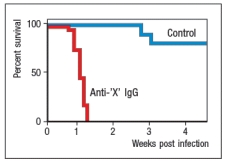 Figure Q10) The most likely candidate for cytokine 'X' is:
Figure Q10) The most likely candidate for cytokine 'X' is:A) IFN-
B) IL-2
C) IL-4
D) IL-17
E) GM-CSF

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
5
Leprosy is a disease caused by the intracellular bacterium Mycobacterium leprae, which infects macrophages and replicates in their phagosomes. Human patients with leprosy have a persistent infection of the mycobacteria, as their immune systems are unable to complete eradicate the pathogen. Furthermore, two different forms of the disease have been identified. Some patients have many skin lesions containing a large number of bacteria with little inflammatory response. This is the very disfiguring form of the disease, and is known as lepromatous leprosy. In other patients, few skin lesions and only occasional bacteria are observed, and the skin lesions are accompanied by a robust inflammatory response. These patients have the form of the disease known as tuberculoid leprosy. If one examined a skin biopsy from a patient with tuberculoid leprosy, one would expect to see:
A) A large influx of neutrophils and other granulocytes
B) A widespread occurrence of tissue necrosis
C) A substantial number of granulomas
D) Evidence of large numbers of dead or dying mycobacteria
E) A large number of skin epithelial cells with intracellular bacteria
A) A large influx of neutrophils and other granulocytes
B) A widespread occurrence of tissue necrosis
C) A substantial number of granulomas
D) Evidence of large numbers of dead or dying mycobacteria
E) A large number of skin epithelial cells with intracellular bacteria

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
6
IL-23 is a cytokine made by macrophages and dendritic cells in response to extracellular bacterial and fungal infections. Mice with a genetic defect in the production of IL-23 are highly susceptible to the gastrointestinal bacterial pathogen, Citrobacter rodentium. Thus, unlike wild-type mice which clear the infection, mice that fail to produce IL-23 succumb to the bacteria and die 1-2 weeks post-infection. Yet, this cytokine does not directly act on the bacteria nor does it function to recruit the granulocytes that are needed to eliminate the pathogen. Instead, IL-23:
A) Functions as a chemoattractant for eosinophils and basophils
B) Stimulates IL-17 and IL-22 production by ILC3 cells
C) Activates tissue-resident ILC2 cells to produce IL-5 and IL-13
D) Induces the differentiation of naive CD8 T cells into cytotoxic T cells
E) Stimulates gastrointestinal epithelial cells to produce antimicrobial peptides
A) Functions as a chemoattractant for eosinophils and basophils
B) Stimulates IL-17 and IL-22 production by ILC3 cells
C) Activates tissue-resident ILC2 cells to produce IL-5 and IL-13
D) Induces the differentiation of naive CD8 T cells into cytotoxic T cells
E) Stimulates gastrointestinal epithelial cells to produce antimicrobial peptides

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
7
Inflammatory bowel disease (colitis) is a CD4 T-cell mediated disease that can be transferred to naive mice by administration of effector CD4 T cells that home to the gastrointestinal tract and induce inflammation. Simultaneous administration of neutralizing antibodies to IL-12p40 can prevent the disease, as can neutralizing antibodies to IL-23p19. Disease symptoms can be exacerbated by administration of IL-23, but not of IL-12. These data strongly suggest that:
A) Both TH1 and TH17 effector cells contribute to disease.
B) TH1 cells producing INF- are the major causes of disease.
C) IL-12p35 is a critical component of disease induction.
D) The inducible IL-12R subunit is essential for disease induction.
E) Neutralizing antibodies to IL-17 would prevent disease.
A) Both TH1 and TH17 effector cells contribute to disease.
B) TH1 cells producing INF- are the major causes of disease.
C) IL-12p35 is a critical component of disease induction.
D) The inducible IL-12R subunit is essential for disease induction.
E) Neutralizing antibodies to IL-17 would prevent disease.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
8
Salmonella typhimurium is a Gram-negative bacterial pathogen that infects its host via the gastrointestinal (GI) tract. Early in infection, the bacteria enter and replicate in gut epithelial cells, where the infection provokes a type 3 response, including the development of TH17 cells, in the GI tract. However, this type 3 response in the GI tract does not eradicate the pathogen, as S. typhimurium has evolved strategies to evade the TH17 response and to spread systemically by infecting and replicating in macrophages. Therefore, a second phase of the immune response is required to completely eliminate the pathogen from the body, as has been demonstrated in mouse models of S. typhimurium infection. These experiments in mouse models likely showed that:
A) IFN- is required to clear S. typhimurium from the body.
B) IL-17 is required to clear S. typhimurium from the body.
C) IL-22 is required to clear S. typhimurium from the body.
D) IL-13 is required to clear S. typhimurium from the body.
E) IL-4 is required to clear S. typhimurium from the body.
A) IFN- is required to clear S. typhimurium from the body.
B) IL-17 is required to clear S. typhimurium from the body.
C) IL-22 is required to clear S. typhimurium from the body.
D) IL-13 is required to clear S. typhimurium from the body.
E) IL-4 is required to clear S. typhimurium from the body.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
9
Allergic airway inflammation can be induced in mice by immunizing them with an allergen that produces a TH2 effector response, and then challenging the immunized mice with an inhaled form of that allergen. In this disease model, the TH2 effector cells present in the lung respond to the inhaled allergen challenge by producing type 2 cytokines that recruit eosinophils and induce airway inflammation. In addition, a component of this TH2 response is antigen-independent, as shown by the effects of administering a neutralizing antibody along with the allergen challenge. This neutralizing antibody (anti-'X' IgG) has the effects shown in Figure Q14).  antibody was shown to inhibit the response of the TH2 cells, and therefore is likely to be:
antibody was shown to inhibit the response of the TH2 cells, and therefore is likely to be:
A) A neutralizing antibody to IL-12
B) A neutralizing antibody to IL-4
C) A neutralizing antibody to TSLP
D) A neutralizing antibody to STAT4
E) A neutralizing antibody to IL-13
 antibody was shown to inhibit the response of the TH2 cells, and therefore is likely to be:
antibody was shown to inhibit the response of the TH2 cells, and therefore is likely to be:A) A neutralizing antibody to IL-12
B) A neutralizing antibody to IL-4
C) A neutralizing antibody to TSLP
D) A neutralizing antibody to STAT4
E) A neutralizing antibody to IL-13

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
10
In addition to producing distinct innate responses locally at the site of infection, the different cytokines produced during type I, type 2, or type 3 immune responses also induce distinct adaptive immune responses that are tailored to the eradication of the three different classes of pathogens. One example is the production of different classes of antibodies during type I, type 2, or type 3 responses. Which step during the induction of the adaptive immune response is the key to generating and coordinating the three different immune modules?

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
11
Immunological memory in humans has been examined by assessing responses in individuals who were given the vaccinia virus to induce immunity against smallpox. Antiviral CD4 and CD8 T cell responses could be detected many years after the vaccinia immunization, but declined with an estimated half-time of about 10 years. In contrast, antiviral antibody responses were maintained at a relatively constant level, with a barely detectable decline over decades. The persistence of antiviral antibodies for years after immunization is likely due to:
A) The presence of CD4 T cell help for memory B cells
B) The presence of long-lived antibody secreting plasma cells
C) The periodic reactivation of memory B cells by low levels of antigen exposure
D) The persistence of the virus in the immunized host
E) The presence of pro-survival cytokines, such as IL-7 and IL-15
A) The presence of CD4 T cell help for memory B cells
B) The presence of long-lived antibody secreting plasma cells
C) The periodic reactivation of memory B cells by low levels of antigen exposure
D) The persistence of the virus in the immunized host
E) The presence of pro-survival cytokines, such as IL-7 and IL-15

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
12
In response to an intracellular bacterial or viral infection, effector TH1 cells, macrophages, NK cells, and CD8 cytotoxic effector cells are all recruited to the site of infection. The coordinated recruitment of all of these cell types is orchestrated by:
A) The secretion of the inflammatory cytokine IFN- in the tissue
B) The action of TNF- on the endothelial cells, leading to fluid leakage into the tissue
C) The up-regulation of integrin ligands such as VLA-4 on the blood vessel endothelial cells
D) The shared expression of chemokine receptors on these different cell types
E) The shared expression of S1PR1 on these cells, recruiting them out of lymphoid tissues
A) The secretion of the inflammatory cytokine IFN- in the tissue
B) The action of TNF- on the endothelial cells, leading to fluid leakage into the tissue
C) The up-regulation of integrin ligands such as VLA-4 on the blood vessel endothelial cells
D) The shared expression of chemokine receptors on these different cell types
E) The shared expression of S1PR1 on these cells, recruiting them out of lymphoid tissues

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
13
Infections of intracellular pathogens (e.g., mycobacteria, listeria, toxoplasma, viruses, etc.) cause a rise in the numbers of monocytes in the blood, a symptom known as monocytosis. In the cases of these infections, monocytosis is likely caused by:
A) Increased production of monocytes in the bone marrow induced by TH1 cytokines
B) Loss of monocytes into tissues due to inflammation, leading to increased production in the bone marrow
C) Differentiation of blood monocytes into macrophages, inducing bone marrow production of new monocytes
D) Sticking of blood monocytes to vessel walls due to integrin binding, reducing the numbers of monocytes in the circulation
E) Apoptosis of monocytes caused by the toxic effects of the infecting pathogen
A) Increased production of monocytes in the bone marrow induced by TH1 cytokines
B) Loss of monocytes into tissues due to inflammation, leading to increased production in the bone marrow
C) Differentiation of blood monocytes into macrophages, inducing bone marrow production of new monocytes
D) Sticking of blood monocytes to vessel walls due to integrin binding, reducing the numbers of monocytes in the circulation
E) Apoptosis of monocytes caused by the toxic effects of the infecting pathogen

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
14
In the cases of some infections, such as mice infected with adenovirus, the generation of effector cytotoxic CD8 T cell responses needed to clear the infection is dependent on the antigen-presenting dendritic cells receiving stimulation through the CD40 receptor on their surface, a process known as dendritic cell 'licensing'. In this infection system, the dendritic cell would likely receive CD40 receptor stimulation from:
A) The activation of a TLR expressed in the dendritic cell
B) The up-regulation of CD40 ligand by virus-infected host cells
C) The activation of cytosolic nucleic acid sensors in the dendritic cell
D) The interaction with a CD4 effector cell expressing CD40 ligand
E) The phagocytosis of apoptotic cell debris resulting from the virus infection
A) The activation of a TLR expressed in the dendritic cell
B) The up-regulation of CD40 ligand by virus-infected host cells
C) The activation of cytosolic nucleic acid sensors in the dendritic cell
D) The interaction with a CD4 effector cell expressing CD40 ligand
E) The phagocytosis of apoptotic cell debris resulting from the virus infection

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
15
Helicobacter pylori is a human gastrointestinal (GI) pathogen that can lead to a state of chronic GI inflammation in some individuals, and has been linked to gastric ulcers and other diseases. Studies have shown that human mucosal gastric biopsies of infected individuals have dendritic cells producing IL-23, and that human monocytes isolated and cultured from healthy individuals produce IL-23, but not IL-12, in response to stimulation with live H. pylori. Given these findings, which of the following responses would be enhanced in the GI tract of H. pylori-infected individuals compared to uninfected individuals?
A) Mucus production by goblet cells
B) Recruitment of neutrophils
C) Recruitment of eosinophils
D) Production of nitric oxide and superoxide
E) Production of IL-13
A) Mucus production by goblet cells
B) Recruitment of neutrophils
C) Recruitment of eosinophils
D) Production of nitric oxide and superoxide
E) Production of IL-13

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
16
While innate immune responses to all types of infections induce local inflammatory responses due to activation of blood vessel endothelial cells, some components of the innate response differ depending on the nature of the pathogen. In the case of intracellular bacterial or protozoan infections, tissue-resident dendritic cells and macrophages produce a cytokine that stimulates ILC cells to produce:
A) IL-13
B) TNF-
C) IL17
D) IL22
E) IFN-
A) IL-13
B) TNF-
C) IL17
D) IL22
E) IFN-

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
17
The kinetics of a typical CD8 T cell response to an acute virus infection in mice is shown in Figure . 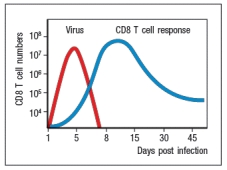 and starting at ~day 10 post-infection, the majority of the virus-specific CD8 T cells die. The death of these virus-specific CD8 T cells is caused by:
and starting at ~day 10 post-infection, the majority of the virus-specific CD8 T cells die. The death of these virus-specific CD8 T cells is caused by:
A) Lysis from the virus infection
B) Engulfment and destruction by phagocytes in the body
C) Destruction by cytotoxic T cells
D) Natural killer cell lysis
E) Fas-induced death or cytokine withdrawal
 and starting at ~day 10 post-infection, the majority of the virus-specific CD8 T cells die. The death of these virus-specific CD8 T cells is caused by:
and starting at ~day 10 post-infection, the majority of the virus-specific CD8 T cells die. The death of these virus-specific CD8 T cells is caused by:A) Lysis from the virus infection
B) Engulfment and destruction by phagocytes in the body
C) Destruction by cytotoxic T cells
D) Natural killer cell lysis
E) Fas-induced death or cytokine withdrawal

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
18
The immune response to helminthic worm infections in the gastrointestinal tract requires specialized mechanisms due to the fact that helminths are too large to be ingested and destroyed by phagocytes. For example, cytokines made by TH2 cells elicit responses from multiple non-hematopoietic cell types that aid in parasite expulsion. Name two of these cell types and for each of them, their response to TH2-produced cytokines.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
19
Individuals with the HIV-induced immunodeficiency disease AIDS have a progressive loss in the number of CD4 T cells in their bodies. These patients have a greatly increased rate of life-threatening disease caused by the inability of their immune system to control infections of the intracellular bacterium, Mycobacterium tuberculosis (Mtb). Mtb infects macrophages and then replicates in the cell's phagosomes. The most important immune mechanism lacking in these patients that leads to their increased susceptibility to Mtb is a defect in:
A) CD4 T cell help for cytotoxic effector CD8 T cells
B) The activation of macrophages by TH1 effector cells
C) The production of opsonizing antibodies that requires TFH cell help for B cells
D) The production of TNF- by the infected macrophages
E) The recruitment of neutrophils to the site of infection
A) CD4 T cell help for cytotoxic effector CD8 T cells
B) The activation of macrophages by TH1 effector cells
C) The production of opsonizing antibodies that requires TFH cell help for B cells
D) The production of TNF- by the infected macrophages
E) The recruitment of neutrophils to the site of infection

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
20
In some infectious diseases, antibodies specific for the pathogen are not essential for clearing a primary infection with that pathogen, but are essential in preventing re-infection by the same pathogen. This protective role of pathogen-specific antibodies is not useful for any clinical applications.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
21
Hyper-IgE syndrome, also known as Job’s syndrome, is an immunodeficiency disease resulting from the lack of function of a single gene (gene ‘X’). Patients with this disease are highly susceptible to infections with extracellular bacteria and fungi, most frequently including Staphylococcus aureus infections and Candida albicans infections in the skin. Analysis of the various immune cell compartments indicates that these patients have normal numbers of each cell lineage (i.e., CD4 and CD8 T cells, B cells, monocytes, dendritic cells, NK cells, granulocytes, etc.), and normal levels of IgG, IgA, and IgM antibodies, but higher than normal levels of IgE.
a) Given this information, name a likely component of the immune response that could be impaired in these patients.
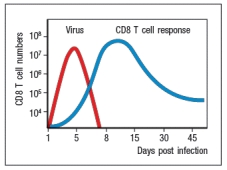
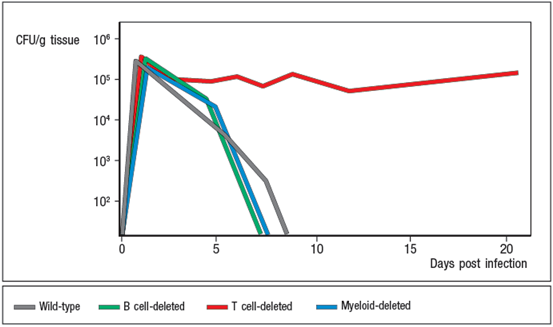
To investigate the immune mechanism impaired in these patients, a mouse model of this gene deficiency was generated. Conditional knockout mouse lines were generated in which gene X was knocked out in either the T cells, the B cells, or the myeloid cells of the mouse. For each conditional knockout line, mice were challenged with Candida albicans, and the ability to clear the infection was assessed. In mice, infection of the oral cavity with Candida albicans has been shown to be a valid model for mucosal Candida albicans infections in humans. After infection, the response was assessed by measuring fungal burden (CFU/g tissue) on the tongue. The resulting data are shown in Figure
b) Based on these data, what is the most likely immune function impaired in the Gene X-deficient patients?
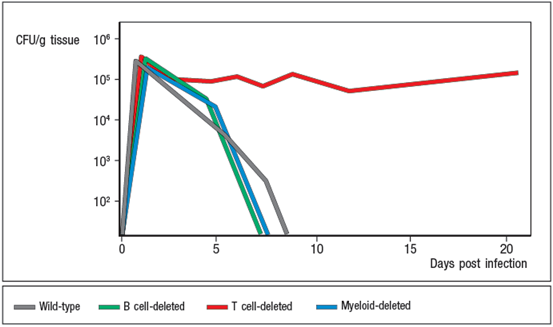
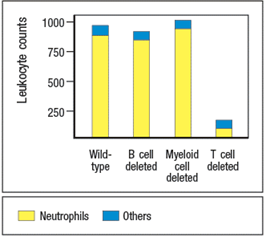
Histological examination of tongue sections from Candida albicans infected mice were examined, and the numbers of infiltrating leukocytes (white blood cells) were quantified in each microscopic field of each section, and the results are shown in Figure
c) Do these data support or refute your hypothesis stated in response to question (b)? Why or why not?
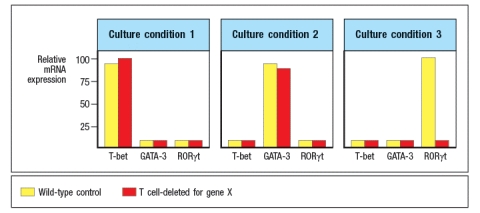
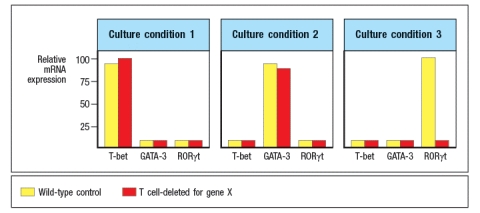
To examine the details of T cell responses when Gene X is absent from the T cells, a series of in vitro experiments were performed. CD4 T cells were isolated from wild type mice and from T cell-deleted Gene X knockout mice, and were stimulated in vitro with a combination of anti-CD3 and anti-CD28 antibodies to activate the T cells. In addition, each culture was supplemented with one of the following cytokine conditions: (1) IFN- plus IL-12; (2) IL-4; or (3) IL-6, TGF- , IL-1 plus IL-23. After four days, the cells were examined for the expression of transcription factors by RT-PCR, as shown in Figure. Note that Gene X does not encode T-bet, GATA-3, or ROR t. Instead, these data indicated impaired responses of Gene X-deficient T cells to the cytokines used in these in vitro culture experiments.
d) Based on these data, name three candidate genes that could be Gene X.
a) Given this information, name a likely component of the immune response that could be impaired in these patients.
To investigate the immune mechanism impaired in these patients, a mouse model of this gene deficiency was generated. Conditional knockout mouse lines were generated in which gene X was knocked out in either the T cells, the B cells, or the myeloid cells of the mouse. For each conditional knockout line, mice were challenged with Candida albicans, and the ability to clear the infection was assessed. In mice, infection of the oral cavity with Candida albicans has been shown to be a valid model for mucosal Candida albicans infections in humans. After infection, the response was assessed by measuring fungal burden (CFU/g tissue) on the tongue. The resulting data are shown in Figure
b) Based on these data, what is the most likely immune function impaired in the Gene X-deficient patients?
Histological examination of tongue sections from Candida albicans infected mice were examined, and the numbers of infiltrating leukocytes (white blood cells) were quantified in each microscopic field of each section, and the results are shown in Figure
c) Do these data support or refute your hypothesis stated in response to question (b)? Why or why not?
To examine the details of T cell responses when Gene X is absent from the T cells, a series of in vitro experiments were performed. CD4 T cells were isolated from wild type mice and from T cell-deleted Gene X knockout mice, and were stimulated in vitro with a combination of anti-CD3 and anti-CD28 antibodies to activate the T cells. In addition, each culture was supplemented with one of the following cytokine conditions: (1) IFN- plus IL-12; (2) IL-4; or (3) IL-6, TGF- , IL-1 plus IL-23. After four days, the cells were examined for the expression of transcription factors by RT-PCR, as shown in Figure. Note that Gene X does not encode T-bet, GATA-3, or ROR t. Instead, these data indicated impaired responses of Gene X-deficient T cells to the cytokines used in these in vitro culture experiments.
d) Based on these data, name three candidate genes that could be Gene X.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
22
Vaccinia virus, used to immunize individuals against smallpox, has a long history of well-documented safe use in humans. Due to the eradication of smallpox, immunizations with vaccinia virus were halted, and babies born after 1970 no longer received this vaccine. This has led to the proposal to engineer vaccinia virus to express proteins derived from other human pathogens for which there are no current vaccines. For instance, the gene encoding the F protein of the respiratory syncytial virus (RSV) has been inserted into vaccinia virus (VaccV-F), and has been tested for its ability to induce anti-F protein antibody responses following immunization.strain if they were born before versus after 1970?

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
23
Studies in mice have shown that resident memory cells (TRM) most often take up permanent residence in the tissue where the initial infection that produced those memory cells occurred. In this location, they are poised to respond rapidly should that infection re-occur in that same location. In contrast, central memory cells (TCM) are primarily found in secondary lymphoid organs, where they can be activated to proliferate and differentiate into effector cells when stimulated by antigen-bearing dendritic cells following re-infection. The third subset of memory cells, effector memory cells (TEM), are recirculating cells that can readily enter tissues at sites of inflammation or infection and are poised to rapidly respond to re-infection. The subset of TEM cells provides an important component of protective immunity to re-infection by the same pathogen because:
A) They are the only memory cell subset that can produce effector cytokines within a few hours of antigen re-encounter.
B) They are able to respond to S1PR1 and enter the blood circulation rapidly upon re-infection.
C) They express the integrin E 7 that binds to integrin ligands expressed on epithelial cells.
D) They can protect against re-infection that occurs in a different site in the body than the primary infection.
E) They can simultaneously express cytokines associated with all three effector T cell lineages.
A) They are the only memory cell subset that can produce effector cytokines within a few hours of antigen re-encounter.
B) They are able to respond to S1PR1 and enter the blood circulation rapidly upon re-infection.
C) They express the integrin E 7 that binds to integrin ligands expressed on epithelial cells.
D) They can protect against re-infection that occurs in a different site in the body than the primary infection.
E) They can simultaneously express cytokines associated with all three effector T cell lineages.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
24
The generation of optimal CD8 T cell memory following a primary infection requires CD4 T cell help for the responding CD8 T cells. This requirement for CD4 T cell help would not be completely replaced by supplying high levels of the cytokine IL-2 during the primary CD8 T cell response.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
25
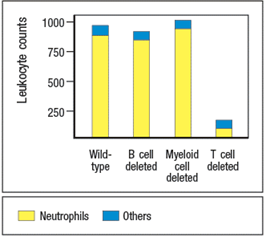
Following an acute virus infection in which the host clears the virus by approximately one week post-infection, a population of virus-specific memory CD8 T cells is maintained and can be detected for months to years post-infection. In mice with a knockout of a single cytokine, virus-specific memory CD8 T cells cannot be maintained, and disappear over time as shown in Figure. 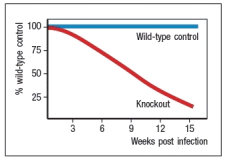
The most likely identity of the cytokine that is missing in these knockout mice is:
A) IL-15
B) IL-2
C) IL-21
D) IL-23
E) IL-4
The most likely identity of the cytokine that is missing in these knockout mice is:
A) IL-15
B) IL-2
C) IL-21
D) IL-23
E) IL-4

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
26
One of the first studies using peptide:MHC class I tetramers to measure the frequencies of virus-specific CD8 T cells in an acute virus infection in mice demonstrated the remarkable finding that more than 50% of all the CD8 T cells in the mouse were virus-specific at the peak of the response (day 8 post-infection). This study used the virus lymphocytic choriomeningitis virus (LCMV). One peptide:MHC tetramer used in this study, H-2-Db loaded with the LCMV nucleoprotein peptide NP396-404, bound to ~20% of the CD8 T cells in the spleen at day 8 post-infection. Why did this tetramer only stain ~20% of the CD8 T cells if more than half of the CD8 cells in the spleen were virus-specific?

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
27
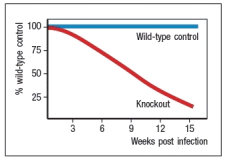
Synthesis question: Leishmania parasites are intracellular protozoa that causes skin sores, and in some individuals, infections that spread systemically and cause damage to internal organs. In mice, different strains of inbred mice have varying responses to the Leishmania parasite Leishmania major. Whereas C57BL/6 mice develop self-healing skin lesions following infection, Balb/c mice develop non-healing lesions and ultimately succumb to systemic, fatal disease. An example of such data is shown in Figure Q28)A. For these studies, mice were infected with 2 106 L. major promastigotes in the footpad, and the sizes of skin lesions and the numbers of parasites per lesion were measured at the indicated times post-infection. 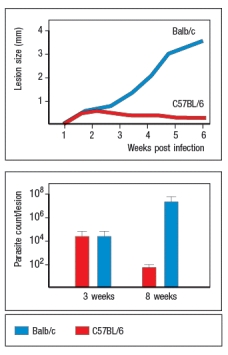 An example of the cytokine data from L. major infected mice is shown in Figure Q28)B. At the indicated times the percentages of CD4 T cells in the draining lymph node producing IFN- versus IL-4 following stimulation with L. major antigens were measured by intracellular cytokine staining.
An example of the cytokine data from L. major infected mice is shown in Figure Q28)B. At the indicated times the percentages of CD4 T cells in the draining lymph node producing IFN- versus IL-4 following stimulation with L. major antigens were measured by intracellular cytokine staining. 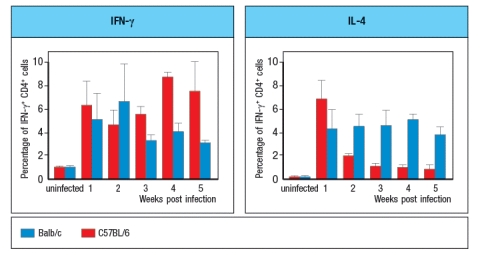
on TH1 effector T cells, CD8 effector T cells, and NK cells. These chemokines are normally not detectable in healthy tissues, but are strongly up-regulated during infection, injury or inflammation, in response to IFN- production in the tissue.
d) How might this information help explain the divergent ability of C57BL/6 versus Balb/c mice to accumulate increasing numbers of effector T cells into the L. major lesions over the long timecourse shown in the data above?
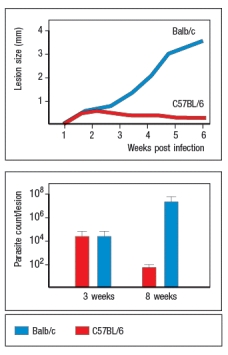 An example of the cytokine data from L. major infected mice is shown in Figure Q28)B. At the indicated times the percentages of CD4 T cells in the draining lymph node producing IFN- versus IL-4 following stimulation with L. major antigens were measured by intracellular cytokine staining.
An example of the cytokine data from L. major infected mice is shown in Figure Q28)B. At the indicated times the percentages of CD4 T cells in the draining lymph node producing IFN- versus IL-4 following stimulation with L. major antigens were measured by intracellular cytokine staining. 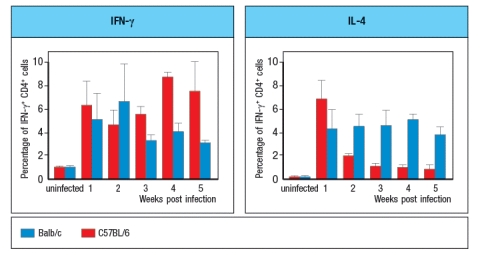
on TH1 effector T cells, CD8 effector T cells, and NK cells. These chemokines are normally not detectable in healthy tissues, but are strongly up-regulated during infection, injury or inflammation, in response to IFN- production in the tissue.
d) How might this information help explain the divergent ability of C57BL/6 versus Balb/c mice to accumulate increasing numbers of effector T cells into the L. major lesions over the long timecourse shown in the data above?

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck
28
It is well documented that antibody affinities for an immunizing antigen continue to increase upon successive rounds of immunization (i.e., secondary, tertiary, etc.). This is due to the fact that:
A) At each round of immunization, new naive B cells are recruited into the response.
B) At each round of immunization, the expression of AID increases, leading to higher rates of somatic hypermutation.
C) Memory B cells express higher levels of AID than naive B cells, leading to higher rates of somatic hypermutation.
D) Memory B cells can re-enter germinal centers and undergo additional somatic hypermutation.
E) At each round of immunization, germinal centers become larger and have increased numbers of B cells in them.
A) At each round of immunization, new naive B cells are recruited into the response.
B) At each round of immunization, the expression of AID increases, leading to higher rates of somatic hypermutation.
C) Memory B cells express higher levels of AID than naive B cells, leading to higher rates of somatic hypermutation.
D) Memory B cells can re-enter germinal centers and undergo additional somatic hypermutation.
E) At each round of immunization, germinal centers become larger and have increased numbers of B cells in them.

Unlock Deck
Unlock for access to all 28 flashcards in this deck.
Unlock Deck
k this deck


