Deck 3: The Induced Responses of Innate Immunity
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/39
Play
Full screen (f)
Deck 3: The Induced Responses of Innate Immunity
1
Dendritic cells are tissue resident myeloid cells that are highly phagocytic, like macrophages. However, dendritic cells do not play a major role in large-scale pathogen destruction; instead, they are important in initiating adaptive immune responses of T cells.
True
2
All mammalian TLRs have been shown to directly bind to microbial products, leading to TLR signaling.
False
3
An infection in the skin, such as a pimple, often produces pus. The major component of pus is:
A) Toxic oxygen molecules released by macrophages
B) Toxic nitrogen molecules released by macrophages
C) NETs released by neutrophils
D) Dead epithelial cells killed by lysozyme
E) Dead and dying neutrophils
A) Toxic oxygen molecules released by macrophages
B) Toxic nitrogen molecules released by macrophages
C) NETs released by neutrophils
D) Dead epithelial cells killed by lysozyme
E) Dead and dying neutrophils
Dead and dying neutrophils
4
Dendritic cells in the skin, known as Langerhans cells, express very high levels of the NOD-like receptor, NLRP3. Previous studies showed that treatment of these cells with the Staphylococcus aureus pore-forming toxin causes K+ efflux from the cells. To investigate whether this signal could induce IL-1 (an inflammatory cytokine) secretion by the cells, the following study was performed: 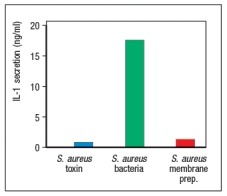
The explanation for these results is:
A) NLRP3 is not activated by K+ efflux from the cells.
B) The S. aureus toxin does not kill the Langerhans cells.
C) The live S. aureus bacteria activate a TLR and NLRP3.
D) The S. aureus membrane prep does not contain a TLR ligand.
E) TLR activation by S. aureus membranes induces interferon production.
The explanation for these results is:
A) NLRP3 is not activated by K+ efflux from the cells.
B) The S. aureus toxin does not kill the Langerhans cells.
C) The live S. aureus bacteria activate a TLR and NLRP3.
D) The S. aureus membrane prep does not contain a TLR ligand.
E) TLR activation by S. aureus membranes induces interferon production.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
5
A key feature of TLR signaling is the ability to induce inflammatory cytokine gene expression extremely rapidly following TLR stimulation. This is accomplished by signaling pathways using several mechanisms to activate transcription factors that are already present in the cell prior to TLR stimulation, but are kept in an inactive state. These signaling pathways use all of the following mechanisms EXCEPT:
A) Induced ubiquitination leading to protein degradation
B) Induced ubiquitination inducing protein-protein interactions
C) Induced phosphorylation leading to nuclear translocation
D) Induced phosphorylation leading to kinase activation
E) Induced phosphorylation preventing protein degradation
A) Induced ubiquitination leading to protein degradation
B) Induced ubiquitination inducing protein-protein interactions
C) Induced phosphorylation leading to nuclear translocation
D) Induced phosphorylation leading to kinase activation
E) Induced phosphorylation preventing protein degradation

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
6
NOD1 and NOD2 are cytoplasmic sensors of bacterial products such as muramyl dipeptide (MDP), a constituent in the peptidoglycans of most bacteria. These sensors are highly expressed in epithelial cells that line the body surfaces that pathogens must cross to establish an infection. Interestingly, a subset of patients with an inflammatory bowel disease called 'Crohn's disease' have inactivating mutations in NOD2. Why might this deficiency in NOD2 lead to chronic inflammation in the gut?

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
7
In recent years, several new vaccines have been developed that are made from purified viral surface proteins, rather than intact or live viruses. They are referred to as subunit vaccines. In order to generate a protective adaptive immune response to a subunit vaccine, the viral protein(s) must be mixed with an adjuvant. The adjuvant functions to:
A) Mimic the process of normal virus entry by binding to the host receptor and inducing receptor-mediated endocytosis
B) Induce vascular permeability to promote the accumulation of fluid and serum proteins at the vaccine injection site
C) Induce the production of chemotactic proteins that recruit neutrophils and then monocytes to the site of vaccine injection
D) Stimulate dendritic cells to up-regulate co-stimulatory molecules and migrate to the regional lymph node
E) Promote the activation of the complement cascade to induce complement deposition on the viral subunit proteins
A) Mimic the process of normal virus entry by binding to the host receptor and inducing receptor-mediated endocytosis
B) Induce vascular permeability to promote the accumulation of fluid and serum proteins at the vaccine injection site
C) Induce the production of chemotactic proteins that recruit neutrophils and then monocytes to the site of vaccine injection
D) Stimulate dendritic cells to up-regulate co-stimulatory molecules and migrate to the regional lymph node
E) Promote the activation of the complement cascade to induce complement deposition on the viral subunit proteins

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
8
When stimulated by binding to bacterial products, the fMet-Leu-Phe (fMLF) receptor triggers multiple responses by phagocytes, including migration and induction of antimicrobial activities. Most of these responses are activated by small GTPases of the Rac and Rho families that are indirectly activated by fMLF receptor stimulation. The fMLF receptor can initiate multiple downstream signaling pathways because:
A) It couples to a heterotrimeric G protein that has and subunits with independent activities.
B) It couples directly to two different guanine nucleotide exchange factors (GEFs).
C) It binds to Rac, Rho, and cdc42 directly.
D) It promotes fusion of phagosomes with lysosomes, initiating multiple signals.
E) It induces assembly of multiple enzymes from individual cytosolic components.
A) It couples to a heterotrimeric G protein that has and subunits with independent activities.
B) It couples directly to two different guanine nucleotide exchange factors (GEFs).
C) It binds to Rac, Rho, and cdc42 directly.
D) It promotes fusion of phagosomes with lysosomes, initiating multiple signals.
E) It induces assembly of multiple enzymes from individual cytosolic components.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
9
Many different NOD-like receptors, including several with pyrin domains and several with HIN domains, can function to trigger inflammasome assembly leading to the activation of caspase-1. The reason for many different sensors in this innate response system is that:
A) Each NOD-like receptor is expressed in a different set of phagocytic cells, depending on its tissue location.
B) Each NOD-like receptor resides in a different intracellular compartment.
C) Each NOD-like receptor performs a different step in the multi-step cascade leading to inflammasome activation.
D) Each NOD-like receptor binds to a different adapter protein and triggers a different form of the inflammasome.
E) Each NOD-like receptor recognizes different PAMPs and is activated by different pathogens.
A) Each NOD-like receptor is expressed in a different set of phagocytic cells, depending on its tissue location.
B) Each NOD-like receptor resides in a different intracellular compartment.
C) Each NOD-like receptor performs a different step in the multi-step cascade leading to inflammasome activation.
D) Each NOD-like receptor binds to a different adapter protein and triggers a different form of the inflammasome.
E) Each NOD-like receptor recognizes different PAMPs and is activated by different pathogens.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
10
Mycobacteria are intracellular pathogens that have adapted to life inside phagocytic cells, such as macrophages. These intracellular bacteria are taken up by phagocytosis, similar to other pathogens, but the bacteria are not killed. One possible mechanism that could account for this immune evasion by mycobacteria is their ability to:
A) Prevent induction of nitric oxide production in the phagosome
B) Prevent the acidification of phagosomes
C) Prevent the expression of antimicrobial peptides in the phagosome
D) Prevent fusion of phagosomes with lysosomes
E) Kill the macrophage before it kills them
A) Prevent induction of nitric oxide production in the phagosome
B) Prevent the acidification of phagosomes
C) Prevent the expression of antimicrobial peptides in the phagosome
D) Prevent fusion of phagosomes with lysosomes
E) Kill the macrophage before it kills them

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
11
RIG-I like receptors (RLRs) such as RIG-I, MDA-5, and STING are cytoplasmic nucleic acid sensors. Give two examples of how such innate sensors distinguish between the RNA/DNA of the host from that of an infecting pathogen.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
12
Most normal tissues contain resident macrophages, and connective tissue sites in the gastrointestinal tract and the lung contain large numbers of these cells. Yet the blood also contains a high number of circulating 'classical' monocytes that can differentiate into macrophages after entering tissues. These circulating monocytes function to:
A) Phagocytose and kill pathogens in the blood
B) Line the endothelial surfaces of the blood vessels with phagocytic cells
C) Enter lymph nodes and patrol for infecting microbes in these organs
D) Amplify the local innate immune response by entering tissues that are infected
E) Differentiate into dendritic cells during an inflammatory response
A) Phagocytose and kill pathogens in the blood
B) Line the endothelial surfaces of the blood vessels with phagocytic cells
C) Enter lymph nodes and patrol for infecting microbes in these organs
D) Amplify the local innate immune response by entering tissues that are infected
E) Differentiate into dendritic cells during an inflammatory response

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
13
Stimulation of the nucleic acid sensing TLRs that reside in endosomal membranes induces the production of a different cytokine response than is produced by stimulation of the plasma membrane TLRs. In part, this distinction is based on the different adapter proteins used by the nucleic acid sensing TLRs, leading to the activation of IRF factors. The cytokine response following stimulation of nucleic acid-sensing TLRs is characterized by production of:
A) The antiviral cytokine, type I interferon
B) TNF- , which induces increased vascular permeability
C) Antimicrobial peptides by macrophages
D) Chemokines that recruit neutrophils
E) The inflammatory complement fragments, C3a and C5a
A) The antiviral cytokine, type I interferon
B) TNF- , which induces increased vascular permeability
C) Antimicrobial peptides by macrophages
D) Chemokines that recruit neutrophils
E) The inflammatory complement fragments, C3a and C5a

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
14
Signaling through the Drosophila Toll pathway is initiated when pathogen recognition receptors (PRRs) bind to microbial products, such as bacterial peptidoglycan. Aspects of this pathway share similarity to the mammalian complement cascade as well as to the innate recognition system based on TLRs. One feature of Toll signaling that resembles the complement pathway is:
A) The activation of an extracellular proteolytic cascade involving cleavage of self-proteins
B) The deposition of Toll signaling proteins onto the microbial surface
C) The release of soluble fragments of Toll that induce inflammation
D) The assembly of a membrane attack complex in the microbial membrane following Toll activation
E) The presence of receptors for Toll cleavage products on phagocytic cells to promote pathogen ingestion
A) The activation of an extracellular proteolytic cascade involving cleavage of self-proteins
B) The deposition of Toll signaling proteins onto the microbial surface
C) The release of soluble fragments of Toll that induce inflammation
D) The assembly of a membrane attack complex in the microbial membrane following Toll activation
E) The presence of receptors for Toll cleavage products on phagocytic cells to promote pathogen ingestion

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
15
As a family, TLRs can recognize PAMPs associated with a broad array of different pathogens, including bacteria, viruses, and fungi. Patients with a specific susceptibility to herpesvirus infections have a defect in their ability to respond to viral nucleic acids using TLR-3, TLR-7, or TLR-9, even though these proteins are expressed in the patients' cells. Analysis of the TLRs in macrophages and dendritic cells from these patients would likely show which of the arrangements in Figure?
A)
B)
C)
D)
E)
A)

B)

C)

D)

E)


Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
16
The NBT (Nitro Blue Tetrazolium) test is used to diagnose the genetic disorder Chronic Granulomatous Disease (CGD). To perform this test, peripheral blood cells from the patient are stimulated with bacterial extracts, and then incubated with the NBT compound. Normal neutrophils turn blue in this test due to cleavage of the compound, while patient neutrophils remain uncolored, as shown in Figure. 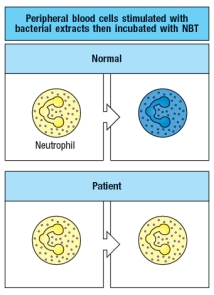
Name a neutrophil receptor that is likely to be stimulated by the bacterial extract in this assay, and describe how this receptor regulates the activity of the enzyme that cleaves NBT.
Name a neutrophil receptor that is likely to be stimulated by the bacterial extract in this assay, and describe how this receptor regulates the activity of the enzyme that cleaves NBT.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
17
The first pattern recognition receptor (PRR) important in innate immune responses was discovered in the fruit fly Drosophila melanogaster. Stimulation of this receptor, called Toll, induces:
A) The synthesis of prostaglandins and leukotrienes
B) The inflammatory response in Drosophila hemolymph vessels
C) The production of antimicrobial peptides
D) The recruitment of phagocytic cells to the site of infection
E) The activation of Drosophila complement
A) The synthesis of prostaglandins and leukotrienes
B) The inflammatory response in Drosophila hemolymph vessels
C) The production of antimicrobial peptides
D) The recruitment of phagocytic cells to the site of infection
E) The activation of Drosophila complement

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
18
Many of the inflammatory mediators produced by tissue macrophages at sites of infection act on the endothelial cells lining the blood vessel walls. An exception to this is (are) the:
A) Cytokines that induce increased vascular permeability
B) Chemokines that induce directed migration of blood monocytes
C) Cytokines that induce increased expression of adhesion molecules
D) TNF produced by tissue-resident sensor cells
E) Bradykinin produced that causes pain
A) Cytokines that induce increased vascular permeability
B) Chemokines that induce directed migration of blood monocytes
C) Cytokines that induce increased expression of adhesion molecules
D) TNF produced by tissue-resident sensor cells
E) Bradykinin produced that causes pain

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
19
The inflammatory response is characterized by four classic symptoms: heat, redness, pain, and swelling. In some instances, this response can be triggered by stimuli that are non-infectious such as asbestos, a process known as 'sterile inflammation.' When exposure to the stimulating trigger is persistent, a state of chronic inflammation can result. This process is likely to be detrimental to the health of the host.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
20
Macrophages express multiple types of receptors on their surface that stimulate phagocytosis of microbes, leading to pathogen internalization and destruction. Many of these receptors, such as Dectin-1, rely on direct recognition of a PAMP on the pathogen surface. However, some receptors that stimulate phagocytosis rely on soluble factors (not associated with the phagocyte membrane) to identify and mark the pathogen for uptake by the phagocyte. One such receptor is:
A) The mannose receptor
B) The class A scavenger receptor
C) The lipid receptor
D) The macrophage C-type lectin receptor
E) The complement receptor
A) The mannose receptor
B) The class A scavenger receptor
C) The lipid receptor
D) The macrophage C-type lectin receptor
E) The complement receptor

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
21
Each family of NK cell receptors has members that promote NK cell activation, and members that send inhibitory signals when engaged. The difference between activating and inhibitory receptors lies in their association with accessory proteins that promote downstream signaling, or in their ability to recruit and activate inhibitory phosphatases, respectively.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
22
In healthy adults, neutrophils represent approximately half of their white blood cells. During a bacterial infection, this number often rises to >80%. One factor contributing to this rise is:
A) Recruitment of neutrophils from tissues into the blood
B) Proliferation of neutrophils at the site of infection
C) Proliferation of neutrophils in the blood
D) Differentiation of blood monocytes into neutrophils
E) Release of neutrophils into the blood from the bone marrow
A) Recruitment of neutrophils from tissues into the blood
B) Proliferation of neutrophils at the site of infection
C) Proliferation of neutrophils in the blood
D) Differentiation of blood monocytes into neutrophils
E) Release of neutrophils into the blood from the bone marrow

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
23
NK cells express receptors from several families, each of which has multiple members. Some of these receptors are activating and others are inhibitory, and NK cell activation is dependent on the balance of signaling overall. The individual NK cells in an individual:
A) Always express a majority of activating versus inhibitory receptors
B) Are more potent effectors of cytotoxicity than of cytokine-production
C) Each express only a subset of all possible NK receptors
D) Are not considered members of the innate lymphoid cell lineage
E) Undergo massive proliferation in response to infection, similar to T lymphocytes
A) Always express a majority of activating versus inhibitory receptors
B) Are more potent effectors of cytotoxicity than of cytokine-production
C) Each express only a subset of all possible NK receptors
D) Are not considered members of the innate lymphoid cell lineage
E) Undergo massive proliferation in response to infection, similar to T lymphocytes

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
24
Many different viruses encode proteins that function to down-regulate MHC class I expression on host cells following infection with the virus. This immune evasion mechanism allows the virus to hide from CD8 T lymphocytes that normally detect virus-infected cells by using their T cell antigen receptor to recognize viral peptides bound to MHC class I proteins on the surface of the infected cell. To counteract this immune evasion strategy, NK cells have:
A) Activating receptors that recognize MHC class I proteins
B) A mechanism to secrete antiviral peptides
C) Inhibitory receptors that recognize viral capsid proteins
D) Activating receptors that recognize viral capsid proteins
E) Inhibitory receptors that recognize MHC class I proteins
A) Activating receptors that recognize MHC class I proteins
B) A mechanism to secrete antiviral peptides
C) Inhibitory receptors that recognize viral capsid proteins
D) Activating receptors that recognize viral capsid proteins
E) Inhibitory receptors that recognize MHC class I proteins

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
25
Immunodeficiency diseases occur when individuals have defects in leukocyte adhesion to inflamed endothelial cells, thereby impeding the extravasation of phagocytes into infected tissues. When neutrophils from one class of these patients were isolated and tested using in vitro assays for neutrophil-endothelial cell interactions and extravasation, it was found that the neutrophils could slowly roll along the endothelial vessel wall but were unable to arrest and migrate across the endothelium. The most likely protein deficient in these neutrophils is:
A) ICAM-1 or ICAM-2
B) P-selectin
C) E-selectin
D) An integrin
E) Sulfated sialyl-LewisX
A) ICAM-1 or ICAM-2
B) P-selectin
C) E-selectin
D) An integrin
E) Sulfated sialyl-LewisX

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
26
To identify genes encoding the receptors for the cytokines IL-2, IL-4, and IL-7, an siRNA screen is performed using purified T lymphocytes. To identify siRNAs that knock-down cytokine receptor expression, the T cells have been transfected with a construct that produces green fluorescent protein (GFP) when any one of these three cytokines is used to stimulate the cells. When the screen is completed, several different siRNAs have been identified that substantially reduce the T cells ability to respond to these cytokines as shown in Figure . 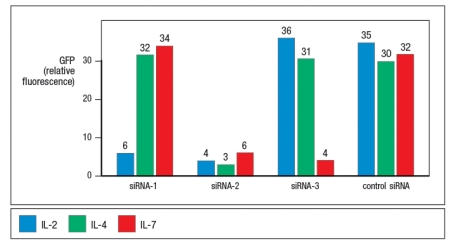
A correct statement regarding these data is:
A) siRNA-1 and siRNA-3 target subunits of the IL-2 receptor but siRNA-2 does not.
B) siRNA-2 targets a shared subunit of all three receptors, whereas siRNA-1 and siRNA-3 do not.
C) siRNA-3 targets a subunit of the IL-7 receptor, but the other two siRNAs do not.
D) siRNA-2 and siRNA-3 do not target a subunit of the IL-2 receptor.
E) siRNA-2 targets a subunit shared by all receptors in the hematopoietin receptor superfamily.
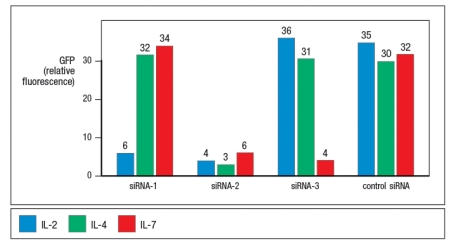
A correct statement regarding these data is:
A) siRNA-1 and siRNA-3 target subunits of the IL-2 receptor but siRNA-2 does not.
B) siRNA-2 targets a shared subunit of all three receptors, whereas siRNA-1 and siRNA-3 do not.
C) siRNA-3 targets a subunit of the IL-7 receptor, but the other two siRNAs do not.
D) siRNA-2 and siRNA-3 do not target a subunit of the IL-2 receptor.
E) siRNA-2 targets a subunit shared by all receptors in the hematopoietin receptor superfamily.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
27
Chemokines such as CXCL8 have a key role in the rapid recruitment of neutrophils to the site in the tissue containing the focus of an infection. In this response, CXCL8 has two different functions. In addition to inducing integrin activation on the neutrophil, CXCL8 also functions to:
A) Induce directional migration of the neutrophil in the tissue
B) Induce increased expression of P-selectin and E-selectin on the endothelium
C) Induce increased expression of integrins on the neutrophil surface
D) Induce blood vessel dilation and fluid leakage into the infected tissue
E) Induce increased phagocytic activity by the neutrophil
A) Induce directional migration of the neutrophil in the tissue
B) Induce increased expression of P-selectin and E-selectin on the endothelium
C) Induce increased expression of integrins on the neutrophil surface
D) Induce blood vessel dilation and fluid leakage into the infected tissue
E) Induce increased phagocytic activity by the neutrophil

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
28
NK cells can be activated following recognition of a virus-infected cell, if that cell has down-regulated expression of MHC class I proteins on its surface. However, NK cells can also recognize infected cells or tumor cells, even if they still express MHC class I proteins. In this latter case, activating receptors on NK cells are recognizing:
A) Molecules on the target cell up-regulated by cellular or metabolic stress
B) Cytokines secreted by the virus-infected or tumor cell
C) MHC class I-like decoy molecules encoded by the virus
D) Mutated self-proteins expressed by the tumor cell
E) Double-stranded DNA in the cytoplasm of the infected or tumor cell
A) Molecules on the target cell up-regulated by cellular or metabolic stress
B) Cytokines secreted by the virus-infected or tumor cell
C) MHC class I-like decoy molecules encoded by the virus
D) Mutated self-proteins expressed by the tumor cell
E) Double-stranded DNA in the cytoplasm of the infected or tumor cell

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
29
Innate lymphoid cells (ILCs) are effector cells that generally reside in barrier tissues, such as the skin, the gut, and the lung. These cells closely resemble subsets of T lymphocytes, but lack a T cell antigen-receptor. Instead, these cells produce their effector molecules following stimulation by:
A) Microbial PAMPs that stimulate pattern recognition receptors on ILCs
B) TNF- , which is produced during the inflammatory response
C) Acute phase response proteins produced in the liver during an infection
D) Cytokines made by other innate cells, such as macrophages or dendritic cells
E) Antimicrobial peptides made by epithelial cells in response to infection
A) Microbial PAMPs that stimulate pattern recognition receptors on ILCs
B) TNF- , which is produced during the inflammatory response
C) Acute phase response proteins produced in the liver during an infection
D) Cytokines made by other innate cells, such as macrophages or dendritic cells
E) Antimicrobial peptides made by epithelial cells in response to infection

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
30
Chemokines are small chemoattractant molecules made by epithelial cells, tissue macrophages, and endothelial cells in response to infection or injury. They differ slightly in sequence and structure based on the cells that secrete them, but all of them act to recruit both monocytes and neutrophils from the blood.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
31
The extravasation of neutrophils into tissues at sites of infection or inflammation requires changes to both the endothelium and to the neutrophil that are induced by chemokines and cytokines produced in the infected tissue.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
32
Two strains of mice were infected with 5 104 PFU of Influenza A virus, and the survival data shown in Figure were obtained. 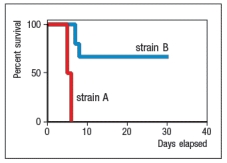
Next, both strains were infected again with Influenza A, and levels of type I interferons (IFN- and IFN- ) were measured and found to be similar between the two strains. Likewise, cells from both strains expressed similar levels of the IFN- / receptor (IFNAR). Which of the following proteins might be more highly expressed in strain B than in strain A following Influenza A infection?
A) MHC class I
B) Mx-1
C) TLR4
D) Complement C3
E) ICAM-1
Next, both strains were infected again with Influenza A, and levels of type I interferons (IFN- and IFN- ) were measured and found to be similar between the two strains. Likewise, cells from both strains expressed similar levels of the IFN- / receptor (IFNAR). Which of the following proteins might be more highly expressed in strain B than in strain A following Influenza A infection?
A) MHC class I
B) Mx-1
C) TLR4
D) Complement C3
E) ICAM-1

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
33
The acute phase response contributes to infection control by producing molecules that promote pathogen opsonization and complement activation. This response is only induced by direct action of microbial components on hepatocytes in the liver.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
34
Cytokine receptors of the hematopoietin superfamily engage signaling pathways that begin with JAK kinases and lead to activation of STAT-family transcription factors. Each receptor subunit in this superfamily binds a specific JAK kinase (one of four members) and each receptor complex usually activates one major STAT homodimer (one of seven). The specificity for activation of one STAT homodimer by each cytokine is determined by:
A) The specificity of each JAK kinase for only phosphorylating one or two out of the seven possible STAT members
B) The specificity of each cytokine receptor complex to only activate one of the four Jak kinase members, which then homodimerizes
C) The amino acid sequence surrounding the phosphorylated tyrosine on each cytokine receptor subunit's cytoplasmic tail
D) The expression of only one STAT member in each type of immune cell, depending on which cytokine receptors are expressed
E) The inhibition of all but one STAT protein by the inhibitor SOCS proteins expressed in each cell type
A) The specificity of each JAK kinase for only phosphorylating one or two out of the seven possible STAT members
B) The specificity of each cytokine receptor complex to only activate one of the four Jak kinase members, which then homodimerizes
C) The amino acid sequence surrounding the phosphorylated tyrosine on each cytokine receptor subunit's cytoplasmic tail
D) The expression of only one STAT member in each type of immune cell, depending on which cytokine receptors are expressed
E) The inhibition of all but one STAT protein by the inhibitor SOCS proteins expressed in each cell type

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
35
Septic shock is a serious, often fatal response to an infection in the bloodstream. This response can be elicited in mice by intravenous injection of bacterial LPS. However, it was found that one strain of mice, C3H/HeJ, is resistant to LPS-induced shock. This fact was used to clone the gene for TLR-4 based on positional cloning from C3H/HeJ mice. Another example of a strain of mice that is resistant to LPS-induced septic shock is:
A) TNF-receptor-deficient mice
B) TLR-2-deficient mice.
C) LFA-1-deficient mice
D) Neutrophil-deficient mice
E) Complement receptor-deficient mice
A) TNF-receptor-deficient mice
B) TLR-2-deficient mice.
C) LFA-1-deficient mice
D) Neutrophil-deficient mice
E) Complement receptor-deficient mice

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
36
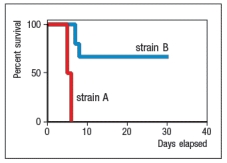
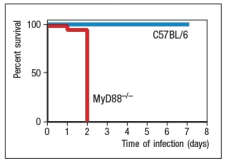
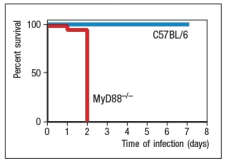
Streptococcus pyogenes is a Group A Streptococcal (GAS) bacterium that causes a variety of diseases, depending on the tissue that is infected. Most frequently, this bacterium causes strep throat and localized infections in the skin. However, on occasion, the bacteria spread to the blood, and can a cause life-threatening infection that has a mortality rate of ~25%. Studies in mouse models have shown that the recruitment of neutrophils to the site of infection is essential in the efficient elimination of a Group A strep infection. To determine the innate immune pathways involved in protection against GAS, mice lacking the adapter protein MyD88 were tested for their response to GAS compared with wild-type (C57BL/6) control mice. For these studies, mice were infected with 104 PFU of GAS subcutaneously (under the skin). The results are shown in Figure.
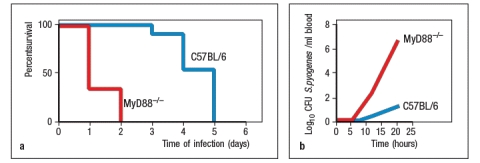
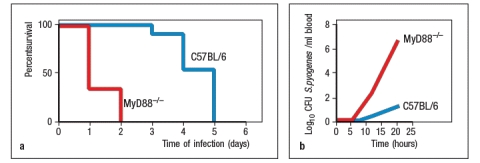
To assess the magnitude of the increased susceptibility of MyD88-/- mice to GAS, mice were tested with increasing doses of bacteria, and the LD50 (dose required to generate a lethal infection in 50% of the mice) was calculated. The conclusion of this analysis was an LD50 of 2 106 PFU for the wild-type mice, and <1 104 for the MyD88-/- mice. In addition, when mice were infected with 5 107 PFU of GAS subcutaneously, as shown in Figure panel A, all the mice eventually succumbed to the infection, but the average survival time of the wild-type mice was significantly longer than for the MyD88-/- mice. In addition, measurements of bacterial counts in the blood within the first day post-infection (panel B) confirmed the poor innate immune response of the MyD88-/- mice.
However, when various knockouts of individual TLRs were tested, none of them showed increased susceptibility to GAS of a magnitude similar to the MyD88-/- mice; similarly, double knockouts of several TLRs in various combinations also failed to recapitulate the severe defect in innate immune response observed in the absence of MyD88.
a) Propose an explanation for the importance of MyD88 in the innate immune response to GAS.
b) If TLRs are not required for the innate immune response to GAS, what other sensor of bacterial components is a good candidate to induce the transcription of pro-inflammatory cytokine genes?
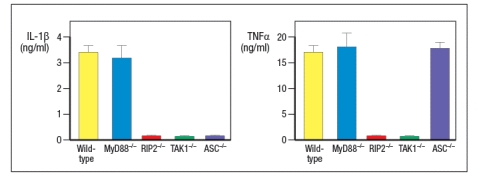
To investigate the innate immune response to GAS further, macrophages were isolated from mice, and cultured together with live GAS bacteria. In addition to macrophages from wild-type mice, macrophages were also isolated from MyD88-/-, RIP2-/-, TAK1-/- and ASC-/- mice. After 18 hours of incubation, the supernatants from these cultures were test for IL-1 and TNF- concentrations. The results are shown in Figure C.signaling; RIP2 for NOD receptor signaling; TAK1 for TLR and NOD receptor signaling; ASC for NLRP3 signaling to activate Caspase-1)
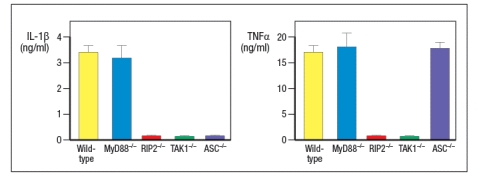
c) Based on these data, what can you conclude about the function of MyD88 in the innate response to GAS?
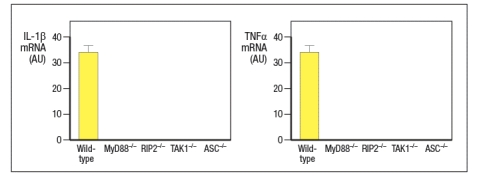
d) On the graphs in Figure , draw the expected results for IL-1β and TNF- mRNA levels in these macrophages. The results from wild-type macrophages are shown for reference.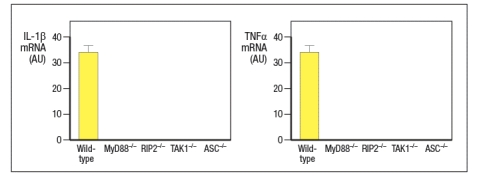
To assess the magnitude of the increased susceptibility of MyD88-/- mice to GAS, mice were tested with increasing doses of bacteria, and the LD50 (dose required to generate a lethal infection in 50% of the mice) was calculated. The conclusion of this analysis was an LD50 of 2 106 PFU for the wild-type mice, and <1 104 for the MyD88-/- mice. In addition, when mice were infected with 5 107 PFU of GAS subcutaneously, as shown in Figure panel A, all the mice eventually succumbed to the infection, but the average survival time of the wild-type mice was significantly longer than for the MyD88-/- mice. In addition, measurements of bacterial counts in the blood within the first day post-infection (panel B) confirmed the poor innate immune response of the MyD88-/- mice.
However, when various knockouts of individual TLRs were tested, none of them showed increased susceptibility to GAS of a magnitude similar to the MyD88-/- mice; similarly, double knockouts of several TLRs in various combinations also failed to recapitulate the severe defect in innate immune response observed in the absence of MyD88.
a) Propose an explanation for the importance of MyD88 in the innate immune response to GAS.
b) If TLRs are not required for the innate immune response to GAS, what other sensor of bacterial components is a good candidate to induce the transcription of pro-inflammatory cytokine genes?
To investigate the innate immune response to GAS further, macrophages were isolated from mice, and cultured together with live GAS bacteria. In addition to macrophages from wild-type mice, macrophages were also isolated from MyD88-/-, RIP2-/-, TAK1-/- and ASC-/- mice. After 18 hours of incubation, the supernatants from these cultures were test for IL-1 and TNF- concentrations. The results are shown in Figure C.signaling; RIP2 for NOD receptor signaling; TAK1 for TLR and NOD receptor signaling; ASC for NLRP3 signaling to activate Caspase-1)
c) Based on these data, what can you conclude about the function of MyD88 in the innate response to GAS?
d) On the graphs in Figure , draw the expected results for IL-1β and TNF- mRNA levels in these macrophages. The results from wild-type macrophages are shown for reference.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
37
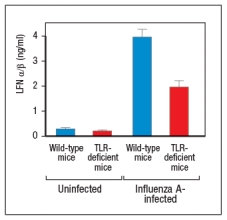
Influenza virus infects and replicates in airway epithelial cells. This virus has a segmented single-stranded RNA genome. Experiments to determine which innate immune sensors were recognizing the virus and inducing production of type I IFNs (IFN- and IFN- ) were performed. For these studies, mice were infected with Influenza A virus by the intranasal route, which leads to a potent infection in the lungs. Two days post-infection, Type I IFNs were measured in the lung; A shows the results. 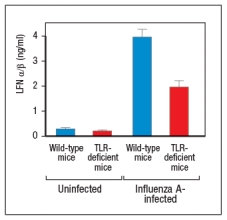
a) Name two innate sensor categories that are likely involved in recognizing influenza virus.
b) A common symptom of virus infections is fever. Which innate receptor sensing pathway is most likely responsible for this response, and how is it induced?
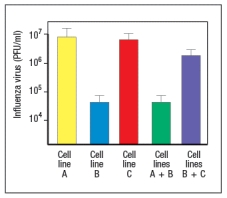
Several cell culture lines of epithelial cells, called "Cell Line A, B, or C," are incubated with 104 infectious particles of influenza virus, and viral titers in the culture media are measured 2 days later. Looking at the results of this experiment, it is apparent that the three lines do not all show the same response to the virus. To investigate these differences, mixing experiments are performed, where cells from two different cell lines are mixed together at a 1:1 ratio before the Influenza infection.
c) Based on the results shown in Figure , propose an explanation for these data.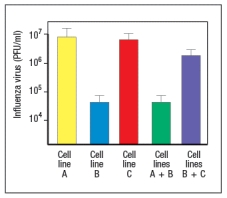
a) Name two innate sensor categories that are likely involved in recognizing influenza virus.
b) A common symptom of virus infections is fever. Which innate receptor sensing pathway is most likely responsible for this response, and how is it induced?
Several cell culture lines of epithelial cells, called "Cell Line A, B, or C," are incubated with 104 infectious particles of influenza virus, and viral titers in the culture media are measured 2 days later. Looking at the results of this experiment, it is apparent that the three lines do not all show the same response to the virus. To investigate these differences, mixing experiments are performed, where cells from two different cell lines are mixed together at a 1:1 ratio before the Influenza infection.
c) Based on the results shown in Figure , propose an explanation for these data.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
38
Individuals with natural killer (NK) cell deficiencies have susceptibilities to infections with herpesviruses and other DNA viruses, as well as with intracellular bacteria such as the mycobacteria that cause tuberculosis. Mycobacterium tuberculosis is a pathogen that infects macrophages and replicates in their phagocytic vesicles. Which effector function of NK cells is likely most important in promoting immunity to M. tuberculosis?

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck
39
In the sea urchin, a massive diversification of innate recognition receptors has occurred, resulting in the presence of over 200 TLR genes, over 200 NOD-like receptor genes, and over 200 scavenger receptor genes in the genome of these organisms. These receptors are unlikely to contribute to an enhanced innate immune response in sea urchins, because nearly all of these genes are pseuodgenes.

Unlock Deck
Unlock for access to all 39 flashcards in this deck.
Unlock Deck
k this deck


