
Biomedical Engineering: Bridging Medicine and Technology 1st Edition by Veronique Tran,Mark Saltzman
Edition 1ISBN: 9780521840996
Biomedical Engineering: Bridging Medicine and Technology 1st Edition by Veronique Tran,Mark Saltzman
Edition 1ISBN: 9780521840996 Exercise 5
One of the major limitations in tissue engineering is vascularization. Without
an adequate blood supply, most grafted tissues will suffer tremendously. In
fact, most researchers in this field would argue that this is the single most
significant hurdle that must be overcome for us to achieve overwhelming
success. Even if we can establish conditions that support the proliferation and
differentiation of three-dimensional tissue-engineered constructs in vitro, the
survival of these constructs after implantation will be unlikely unless there is
an adequate supply of blood. The liver, in particular, requires a very large sup-
ply of blood for its survival. Currently, polyglycolic acid (PGA)/hepatocyte
constructs are grown in culture then implanted into the mesentery of the
rat for in vivo studies. The mesentery is a highly vascularized membranous
fold that attaches the small intestine to the dorsal wall of the body. Despite
this highly vascularized bed for implantation, the present survival rate of
implanted hepatocytes is very low. There is research underway to improve
the vascularization of implanted hepatocytes for replacement of the liver:
• In one case, researchers are impregnating the PGA scaffold with VEGF, a
growth factor that induces the growth of new blood vessels (angiogenesis).
• In a second case, researchers are using advanced free-form fabrication
techniques to create a three-dimensional polymer structure that looks like
a capillary bed.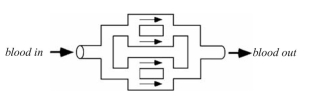
The hepatocytes would be seeded on the exterior of the capillary bed structure.
The two ends of the structure can then be sutured directly in line with a blood
vessel. The device would NOT be encased within any other membrane (i.e., this
is an open system). From the information given here, from our discussions in
class, and considering the many functions of the liver, thoroughly discuss the
following:
a. What would be the major concerns with each approach and why?
b. What would be the major advantages to each approach and why?
an adequate blood supply, most grafted tissues will suffer tremendously. In
fact, most researchers in this field would argue that this is the single most
significant hurdle that must be overcome for us to achieve overwhelming
success. Even if we can establish conditions that support the proliferation and
differentiation of three-dimensional tissue-engineered constructs in vitro, the
survival of these constructs after implantation will be unlikely unless there is
an adequate supply of blood. The liver, in particular, requires a very large sup-
ply of blood for its survival. Currently, polyglycolic acid (PGA)/hepatocyte
constructs are grown in culture then implanted into the mesentery of the
rat for in vivo studies. The mesentery is a highly vascularized membranous
fold that attaches the small intestine to the dorsal wall of the body. Despite
this highly vascularized bed for implantation, the present survival rate of
implanted hepatocytes is very low. There is research underway to improve
the vascularization of implanted hepatocytes for replacement of the liver:
• In one case, researchers are impregnating the PGA scaffold with VEGF, a
growth factor that induces the growth of new blood vessels (angiogenesis).
• In a second case, researchers are using advanced free-form fabrication
techniques to create a three-dimensional polymer structure that looks like
a capillary bed.
The hepatocytes would be seeded on the exterior of the capillary bed structure.
The two ends of the structure can then be sutured directly in line with a blood
vessel. The device would NOT be encased within any other membrane (i.e., this
is an open system). From the information given here, from our discussions in
class, and considering the many functions of the liver, thoroughly discuss the
following:
a. What would be the major concerns with each approach and why?
b. What would be the major advantages to each approach and why?
Explanation
Vascularization is the process of becomi...
Biomedical Engineering: Bridging Medicine and Technology 1st Edition by Veronique Tran,Mark Saltzman
Why don’t you like this exercise?
Other Minimum 8 character and maximum 255 character
Character 255


