Deck 13: Injections for Palatal Pain Control
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
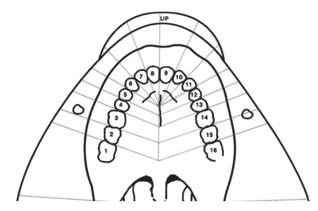
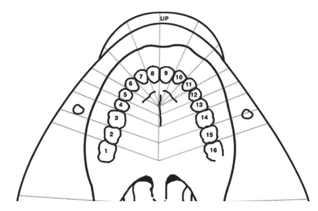
Question
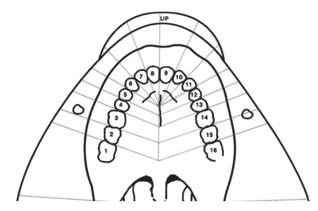
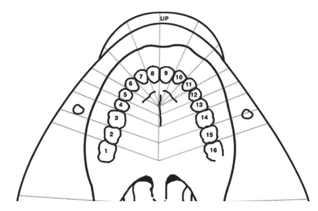
Question
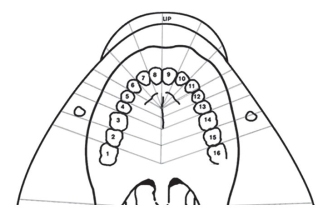
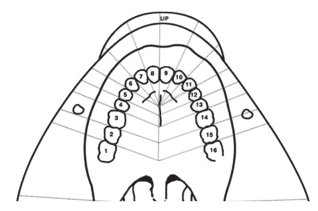
Question
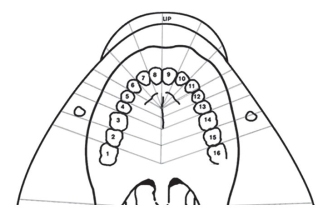
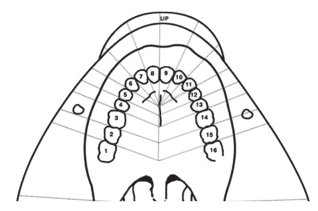
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/73
Play
Full screen (f)
Deck 13: Injections for Palatal Pain Control
1
The nasopalatine nerve is a terminal and short branch of the PSA nerve.
False
2
Excessive blanching more commonly occurs when administering solutions that contain vasoconstrictors.
True
3
The GP nerve branches from the maxillary nerve within the pterygopalatine fossa and is anesthetized by a GP nerve block just prior to its entrance to the pterygopalatine canal.
False
4
The gate control theory suggests that pressure anesthesia blocks the stimulation of non-nociceptive fibers.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
5
The rate of deposition of solution for all palatal injections should be 0.4 mL over 40 seconds.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
6
It should take twice the time to deposit a cartridge of a 4% local anesthetic solution compared to a 2% solution.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
7
For palatal injections, if swelling or blanching occurs, withdraw the needle and choose another penetration site.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
8
A nasopalatine nerve block will anesthetize palatal soft and osseous tissue in the anterior third of the palate, from canine to canine.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
9
The optimum penetration site for the NP nerve block is adjacent to the narrowest portion of the incisive papilla to facilitate ease of insertion.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
10
The P-ASA injection successfully anesthetizes bilateral nasopalatine and ASA nerves.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
11
A P-ASA injection requires a 27 gauge long needle due to the increased depth of insertion.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
12
The field of anesthesia for a P-ASA injection includes the same structures that are innervated by the right and left NP and anterior branches of the ASA nerves.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
13
The rate of deposition of anesthetic solution is the same for the NP and P-ASA injections.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
14
The AMSA injection does not anesthetize labial tissues.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
15
The rate of deposition for an AMSA injection is 0.4 mL over 40 seconds.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
16
The penetration site for a GP injection is in the fossa located anterior to the GP foramen (also referred to as the anterior depression).

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
17
Anesthesia of the soft palate is common because the lesser palatine nerve and foramen are located immediately posterior to the greater palatine foramen.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
18
The needle pathway for a GP nerve block is 6 to 8 mm through dense mucosal tissue.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
19
An extra short needle is not used for GP nerve blocks due to the penetration location at a more posterior position in the palate.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
20
The two-step method for pre-anesthesia for palatal injections includes a one-minute application of topical anesthesia and ________.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
21
Topical anesthetic patches may provide a ________ depth of anesthetic penetration.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
22
The nasopalatine nerve is the longest branch of the posterior superior nasal branch of the ________ nerve.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
23
The ________ theory explains why pressure anesthesia is effective in palatal nerve blocks.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
24
In order to avoid discomfort during palatal injections, the ________ is reduced.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
25
Computer-controlled local anesthetic devises (CCLAD) are ideal for palatal nerve blocks because they provide electronically regulated ________ recommended for all palatal injections.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
26
P-ASA and AMSA nerve blocks are advantageous for cosmetic procedures because anesthesia of the ________ is typically avoided.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
27
Rapid deposition of anesthetic solutions containing vasoconstrictors should be avoided to prevent ________.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
28
The use of 4% anesthetic solutions in the palate should be accompanied by very __________ depositions.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
29
Which one of the following is the most important consideration for palatal local anesthetic procedures?
A) Apply topical anesthetic for one to two minutes
B) Use ester topical anesthetic drug
C) Administer solution slowly
D) Withdraw the needle if swelling and ischemia occur
A) Apply topical anesthetic for one to two minutes
B) Use ester topical anesthetic drug
C) Administer solution slowly
D) Withdraw the needle if swelling and ischemia occur

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
30
Which statement correctly describes one precaution when using 4% local anesthetic drugs for palatal injections?
A) Deposit 0.4 mL over forty seconds
B) Deposit approximately twice as slowly as for 2% solutions
C) Use a 4% solution without a vasoconstrictor
D) Do not use 4% local anesthetic drugs for palatal injections
A) Deposit 0.4 mL over forty seconds
B) Deposit approximately twice as slowly as for 2% solutions
C) Use a 4% solution without a vasoconstrictor
D) Do not use 4% local anesthetic drugs for palatal injections

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
31
The most common cause of failure of palatal nerve blocks is:
A) Solution deposited too far from deposition site
B) Solution deposited too rapidly and it backflows into the mouth
C) Vasoconstrictor constricts the vessels preventing the flow of solution to the nerve
D) Inadequate topical and pressure anesthesia prevent adequate penetration depth
A) Solution deposited too far from deposition site
B) Solution deposited too rapidly and it backflows into the mouth
C) Vasoconstrictor constricts the vessels preventing the flow of solution to the nerve
D) Inadequate topical and pressure anesthesia prevent adequate penetration depth

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
32
Which of the following nerve branches anesthetizes the upper lip and skin of the cheek?
A) Facial nerve
B) Trigeminal nerve, division 1
C) Trigeminal nerve, division 2
D) Trigeminal nerve, division 3
A) Facial nerve
B) Trigeminal nerve, division 1
C) Trigeminal nerve, division 2
D) Trigeminal nerve, division 3

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
33
Which of the following statements is true of the NP nerve block?
A) Provides highest rate of positive aspiration of palatal injections
B) Provides more durable anesthesia than other palatal injections
C) Provides bilateral anesthesia
D) Contact with bone should be avoided
A) Provides highest rate of positive aspiration of palatal injections
B) Provides more durable anesthesia than other palatal injections
C) Provides bilateral anesthesia
D) Contact with bone should be avoided

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
34
Which one of the following is not anesthetized by a nasopalatine nerve block?
A) Soft tissues of the anterior one third of the palate
B) Lingual gingiva, canine to canine
C) Maxillary incisors and canines
D) Incisive papilla
A) Soft tissues of the anterior one third of the palate
B) Lingual gingiva, canine to canine
C) Maxillary incisors and canines
D) Incisive papilla

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
35
Which location represents the correct penetration site for a nasopalatine nerve block?
A) Palatal mucosa lateral to the widest anteroposterior dimension of the incisive papilla
B) Palatal mucosa at the base of the incisive papilla on the right or left side of the incisive papilla
C) Midline in the incisive papilla at the widest anteroposterior dimension of the incisive papilla
D) Perpendicular to the incisive papilla at the widest dimension
A) Palatal mucosa lateral to the widest anteroposterior dimension of the incisive papilla
B) Palatal mucosa at the base of the incisive papilla on the right or left side of the incisive papilla
C) Midline in the incisive papilla at the widest anteroposterior dimension of the incisive papilla
D) Perpendicular to the incisive papilla at the widest dimension

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
36
Which of the following represents the correct penetration depth for a nasopalatine nerve block?
A) 2 to 3 mm
B) 4 to 7 mm
C) 6 to 12 mm
D) 10 to 16 mm
A) 2 to 3 mm
B) 4 to 7 mm
C) 6 to 12 mm
D) 10 to 16 mm

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
37
Which statement describing the injection steps for a nasopalatine nerve block is not correct?
A) Use a two-step pre-anesthesia method
B) Penetrate parallel to the incisive canal until bone is contracted
C) After contacting bone, withdraw 1 mm
D) Deposit solution at a rate of 0.4 mL over forty seconds
A) Use a two-step pre-anesthesia method
B) Penetrate parallel to the incisive canal until bone is contracted
C) After contacting bone, withdraw 1 mm
D) Deposit solution at a rate of 0.4 mL over forty seconds

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
38
What is the most likely cause of unilateral failure of a nasopalatine nerve block?
A) Use of an extra-short needle
B) Inadequate volume of anesthesia
C) Opposite wall of canal is not contacted with needle
D) Backflow of solution along the needle pathway
A) Use of an extra-short needle
B) Inadequate volume of anesthesia
C) Opposite wall of canal is not contacted with needle
D) Backflow of solution along the needle pathway

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
39
Which of the following is the best indication of a P-ASA nerve block?
A) Pain management of palatal tissue
B) Pain management for extensive restorative therapy
C) Pain management for cosmetic dental procedures
D) Pain management for anterior facial and lingual soft tissues
A) Pain management of palatal tissue
B) Pain management for extensive restorative therapy
C) Pain management for cosmetic dental procedures
D) Pain management for anterior facial and lingual soft tissues

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
40
Which structures are not anesthetized by the P-ASA nerve block?
A) Facial and palatal soft and hard tissues associated with the teeth and the pulps of the teeth canine to canine
B) Structures anesthetized by right and left MSA nerve blocks
C) Structures innervated by the right and left nasopalatine nerves
D) Structures innervated by the right and left anterior branches of the ASA nerves
A) Facial and palatal soft and hard tissues associated with the teeth and the pulps of the teeth canine to canine
B) Structures anesthetized by right and left MSA nerve blocks
C) Structures innervated by the right and left nasopalatine nerves
D) Structures innervated by the right and left anterior branches of the ASA nerves

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
41
Which statement best describes the needle pathway for a P-ASA nerve block?
A) Advance needle to a depth of 6 to 10 mm in the center of the canal
B) Advance needle to a depth of 4 to 6 mm within the canal
C) Advance needle parallel to the long axis of the central incisors to a depth of 6 to 10 mm into the canal
D) Using the wall of the canal as a guide, advance needle parallel to the long axis of the central incisors to depth of 6 to 10 mm into the canal
A) Advance needle to a depth of 6 to 10 mm in the center of the canal
B) Advance needle to a depth of 4 to 6 mm within the canal
C) Advance needle parallel to the long axis of the central incisors to a depth of 6 to 10 mm into the canal
D) Using the wall of the canal as a guide, advance needle parallel to the long axis of the central incisors to depth of 6 to 10 mm into the canal

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
42
What is the correct penetration depth for a P-ASA nerve block?
A) 2 to 6 mm
B) 2 to 10 mm
C) 4 to 6 mm
D) 6 to 10 mm
A) 2 to 6 mm
B) 2 to 10 mm
C) 4 to 6 mm
D) 6 to 10 mm

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
43
Which needle is commonly used for a P-ASA nerve block?
A) 25 gauge short
B) 27 gauge long
C) 27 gauge short
D) 25 gauge extra short
A) 25 gauge short
B) 27 gauge long
C) 27 gauge short
D) 25 gauge extra short

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
44
What is the correct deposition rate for the P-ASA nerve bock?
A) 0.5 mL over 60 seconds
B) 0.5 mL over 90 seconds
C) 1.8 mL over 1 minute
D) 1.8 mL over 2 minutes
A) 0.5 mL over 60 seconds
B) 0.5 mL over 90 seconds
C) 1.8 mL over 1 minute
D) 1.8 mL over 2 minutes

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
45
What is the typical minimum volume of anesthetic solution deposited for P-ASA nerve blocks?
A) 0.5 to 1.0 mL
B) 0.9 to 1.8 mL
C) 1.4 to 1.8 mL
D) 1.0 mL
A) 0.5 to 1.0 mL
B) 0.9 to 1.8 mL
C) 1.4 to 1.8 mL
D) 1.0 mL

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
46
What nerve branch can provide assessory innervation causing incomplete anesthesia following a P-ASA nerve block?
A) Facial nerve branch
B) Nasal nerve branch
C) MSA nerve
D) Greater palatine
A) Facial nerve branch
B) Nasal nerve branch
C) MSA nerve
D) Greater palatine

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
47
Which of the following best describes the nerves anesthetized by the AMSA nerve block?
A) GP, MSA, NP
B) NP, ASA, MSA
C) NP, ASA, MSA, PSA
D) ASA, MSA, NP, GP
A) GP, MSA, NP
B) NP, ASA, MSA
C) NP, ASA, MSA, PSA
D) ASA, MSA, NP, GP

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
48
Which of the following is not a clinical advantage of the AMSA nerve block?
A) No anesthesia of associated labial tissues for cosmetic procedures
B) Profound pulpal anesthesia of maxillary first molar
C) Less total drug volume administered
D) Requires one needle penetration
A) No anesthesia of associated labial tissues for cosmetic procedures
B) Profound pulpal anesthesia of maxillary first molar
C) Less total drug volume administered
D) Requires one needle penetration

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
49
The field of anesthesia for an AMSA nerve block includes:
A) Pulps of central and lateral incisors, canine, premolars, and molars on the anesthetized side
B) Pulps of central and lateral incisors, canine, and premolars, and upper lip and facial gingival tissues on the anesthetized side
C) Pulps and lingual gingival of the central and lateral incisors, canine, premolars, and molars bilaterally
D) Pulps of the central and lateral incisors, canine, and premolars, and palatal tissues from the central incisors through the second molar on the side of injection on the anesthetized side
A) Pulps of central and lateral incisors, canine, premolars, and molars on the anesthetized side
B) Pulps of central and lateral incisors, canine, and premolars, and upper lip and facial gingival tissues on the anesthetized side
C) Pulps and lingual gingival of the central and lateral incisors, canine, premolars, and molars bilaterally
D) Pulps of the central and lateral incisors, canine, and premolars, and palatal tissues from the central incisors through the second molar on the side of injection on the anesthetized side

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
50
What is the optimum site of penetration for an AMSA nerve block?
A) Mucogingival junction between the maxillary premolars
B) Junction between the vertical and horizontal aspects of the palate at an imaginary line drawn from the gingival margin between the maxillary second premolar and the first molar
C) Between the premolars along an imaginary line drawn from the base of the interdental papilla
D) Junction between premolars approximately halfway from the median palatine raphe to the gingival margin
A) Mucogingival junction between the maxillary premolars
B) Junction between the vertical and horizontal aspects of the palate at an imaginary line drawn from the gingival margin between the maxillary second premolar and the first molar
C) Between the premolars along an imaginary line drawn from the base of the interdental papilla
D) Junction between premolars approximately halfway from the median palatine raphe to the gingival margin

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
51
What is a typical minimum volume of anesthetic solution deposited for an AMSA nerve block?
A) 0.2 to 0.6 mL
B) 0.6 to 1.8 mL
C) 0.9 to 1.2 mL
D) 1.2 to 1.8 mL
A) 0.2 to 0.6 mL
B) 0.6 to 1.8 mL
C) 0.9 to 1.2 mL
D) 1.2 to 1.8 mL

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
52
What is the correct deposition rate for an AMSA nerve block?
A) 0.5 mL over 60 seconds
B) 0.3 mL over 40 seconds
C) 0.5 mL over 30 seconds
D) 1.2 mL over 90 seconds
A) 0.5 mL over 60 seconds
B) 0.3 mL over 40 seconds
C) 0.5 mL over 30 seconds
D) 1.2 mL over 90 seconds

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
53
Which of the following statements is the most accurate description of the field of anesthesia for a greater palatine nerve block?
A) Soft and hard palatal tissues unilaterally from the midline
B) Soft and hard palatal tissues bilaterally from the midline
C) Soft and hard palatal tissues unilaterally distal to the canine
D) Soft and hard palatal tissues unilaterally from the canine to the molars
A) Soft and hard palatal tissues unilaterally from the midline
B) Soft and hard palatal tissues bilaterally from the midline
C) Soft and hard palatal tissues unilaterally distal to the canine
D) Soft and hard palatal tissues unilaterally from the canine to the molars

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
54
Terminal fibers of the GP nerve overlap the:
A) Lesser palatine nerves
B) Nasopalatine nerves
C) Anterior superior alveolar nerves
D) Opposite greater palatine nerve
A) Lesser palatine nerves
B) Nasopalatine nerves
C) Anterior superior alveolar nerves
D) Opposite greater palatine nerve

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
55
What is the penetration site for a GP nerve block?
A) Slightly anterior to the greater palatine foramen
B) Greatest depression of the greater palatine foramen
C) Junction of the maxillary and palatal bones medial to an imaginary line drawn between the maxillary first and second premolars
D) Slightly distal to the greater palatine foramen
A) Slightly anterior to the greater palatine foramen
B) Greatest depression of the greater palatine foramen
C) Junction of the maxillary and palatal bones medial to an imaginary line drawn between the maxillary first and second premolars
D) Slightly distal to the greater palatine foramen

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
56
What is the approximate depth of penetration for a GP nerve block?
A) 2 mm
B) 2 to 6 mm
C) 6 to 10 mm
D) 9 to 12 mm
A) 2 mm
B) 2 to 6 mm
C) 6 to 10 mm
D) 9 to 12 mm

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
57
What is a typical minimum dose of anesthetic solution deposited for GP nerve blocks?
A) 1 stopper width (0.2 mL)
B) 2 to 3 stopper widths (0.4 - 0.6 mL)
C) 0.9 to 1.2 mL
D) One-half of a cartridge
A) 1 stopper width (0.2 mL)
B) 2 to 3 stopper widths (0.4 - 0.6 mL)
C) 0.9 to 1.2 mL
D) One-half of a cartridge

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
58
What is the recommended maximum dose of a 4% anesthetic solution for a GP nerve block?
A) 0.3 mL
B) 0.6 mL
C) 0.9 mL
D) 1.2 mL
A) 0.3 mL
B) 0.6 mL
C) 0.9 mL
D) 1.2 mL

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
59
What are the two most important considerations for patient comfort for all palatal local anesthetic procedures?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
60
Explain the gate control theory of pain perception related to the use of pressure anesthesia for palatal injections.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
61
Describe the two-step method of topical anesthesia.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
62
Discuss the procedural modification necessary if excessive tissue blanching and bulging occur when depositing anesthetic solutions for palatal nerve blocks.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
63
Explain the advantages of using P-ASA and AMSA nerve block techniques.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
64
Color in the field of anesthesia and list the structures anesthetized by a nasopalatine nerve block.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
65
Color in the field of anesthesia and list the structures anesthetized by a P-ASA nerve block.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
66
Color in the field of anesthesia and list the structures anesthetized by an AMSA nerve block.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
67
Color in the field of anesthesia and list the structures anesthetized by a GP nerve block.

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
68
The treatment plan for Marjorie Dickens includes crown preparations for teeth #7, #8, and #9.
-Which injection(s) is/are needed for pulpal, facial, and palatal soft tissue anesthesia for #7, #8, and #9 with the least number of needle penetrations planned?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
69
The treatment plan for Marjorie Dickens includes crown preparations for teeth #7, #8, and #9.
-Which other injection choice(s) can be considered if needle penetrations are not limited?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
70
The treatment plan for Marjorie Dickens includes crown preparations for teeth #7, #8, and #9.
-Which needle(s) should be used?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
71
The treatment plan for Jim Martin includes an MOD restoration on tooth #14 requiring rubber dam placement on tooth #15.
-Which injection(s) is/are needed for pulpal and soft tissue anesthesia?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
72
The treatment plan for Jim Martin includes an MOD restoration on tooth #14 requiring rubber dam placement on tooth #15.
-Which needle(s) should be used?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck
73
The treatment plan for Jim Martin includes an MOD restoration on tooth #14 requiring rubber dam placement on tooth #15.
-The gingivopalatal aspect of #14 and #15 has failed to be anesthetized. What is the most common cause(s) for failure of anesthesia following a GP injection?

Unlock Deck
Unlock for access to all 73 flashcards in this deck.
Unlock Deck
k this deck


