Exam 48: Initiating and Adjusting Invasive Ventilatory Support
Exam 1: History of Respiratory Care30 Questions
Exam 2: Delivering Evidence-Based Respiratory Care22 Questions
Exam 3: Quality, Patient Safety, and Communication, and Recordkeeping49 Questions
Exam 4: Principles of Infection Prevention and Control34 Questions
Exam 5: Ethical and Legal Implications of Practice41 Questions
Exam 6: Physical Principles of Respiratory Care88 Questions
Exam 7: E-Medicine in Respiratory Care21 Questions
Exam 8: Fundamentals of Respiratory Care Research10 Questions
Exam 9: The Respiratory System129 Questions
Exam 10: The Cardiovascular System68 Questions
Exam 11: Ventilation78 Questions
Exam 12: Gas Exchange and Transport88 Questions
Exam 13: Solutions, Body Fluids, and Electrolytes94 Questions
Exam 14: Acid-Base Balance100 Questions
Exam 15: Regulation of Breathing50 Questions
Exam 16: Bedside Assessment of the Patient100 Questions
Exam 17: Interpreting Clinical and Laboratory Data38 Questions
Exam 18: Interpreting the Electrocardiogram35 Questions
Exam 19: Analysis and Monitoring of Gas Exchange115 Questions
Exam 20: Pulmonary Function Testing70 Questions
Exam 21: Review of Thoracic Imaging47 Questions
Exam 22: Flexible Bronchoscopy and the Respiratory Therapist25 Questions
Exam 23: Nutrition Assessment46 Questions
Exam 24: Pulmonary Infections56 Questions
Exam 25: Obstructive Lung Disease: Chronic Obstructive Pulmonary Disease Copd, Asthma, and Related Diseases59 Questions
Exam 26: Interstitial Lung Disease45 Questions
Exam 27: Pleural Diseases42 Questions
Exam 28: Pulmonary Vascular Disease57 Questions
Exam 29: Acute Respiratory Distress Syndrome30 Questions
Exam 30: Trauma, Burns and Near Drowning21 Questions
Exam 31: Lung Cancer28 Questions
Exam 32: Neuromuscular and Other Diseases of the Chest Wall29 Questions
Exam 33: Disorders of Sleep30 Questions
Exam 34: Neonatal and Pediatric Respiratory Disorders70 Questions
Exam 35: Airway Pharmacology67 Questions
Exam 36: Airway Management117 Questions
Exam 37: Emergency Cardiovascular Life Support70 Questions
Exam 38: Humidity and Bland Aerosol Therapy109 Questions
Exam 39: Aerosol Drug Therapy116 Questions
Exam 40: Storage and Delivery of Medical Gases78 Questions
Exam 41: Medical Gas Therapy93 Questions
Exam 42: Lung Expansion Therapy63 Questions
Exam 43: Airway Clearance Therapy Act90 Questions
Exam 44: Respiratory Failure and the Need for Ventilatory Support54 Questions
Exam 45: Mechanical Ventilators70 Questions
Exam 46: Physiology of Ventilatory Support89 Questions
Exam 47: Patient Ventilator Interaction22 Questions
Exam 48: Initiating and Adjusting Invasive Ventilatory Support97 Questions
Exam 49: Noninvasive Ventilation51 Questions
Exam 50: Extracorporeal Life Support Ecls25 Questions
Exam 51: Monitoring the Patient in the Intensive Care Unit60 Questions
Exam 52: Discontinuing Ventilatory Support62 Questions
Exam 53: Neonatal and Pediatric Respiratory Care34 Questions
Exam 54: Patient Education and Health Promotion20 Questions
Exam 55: Cardiopulmonary Rehabilitation64 Questions
Exam 56: Respiratory Care in Alternative Settings130 Questions
Select questions type
What is the primary concern when using proning to improve oxygenation in the patient with ARDS?
(Multiple Choice)
4.9/5  (28)
(28)
Which of the following findings would you expect to see in a patient who has acute ventilatory failure with severe hypercapnia?
(Multiple Choice)
4.7/5  (39)
(39)
After setting up a patient on a ventilatory support device, which of the following supplementary equipment would you require to be available at the bedside?
1) Suction source and catheters
2) Backup artificial airway
3) Manual resuscitator with O2
(Multiple Choice)
4.9/5  (34)
(34)
A ventilator has separate rate and minute ventilation controls. A physician orders continuous mandatory ventilation with a VT of 550 ml at a respiratory rate of 12/min. What minute ventilation would you set on this ventilator?
(Multiple Choice)
4.9/5  (48)
(48)
A chronic obstructive pulmonary disease (COPD) patient receiving ventilatory support in the CMV assist-control mode at a rate of 14 and a VT of 750 ml exhibits clinical signs of air trapping. Which of the following would you recommend to correct this problem?
1) Decrease "E" time.
2) Increase the inspiratory flow rate.
3) Decrease the assist-control rate.
(Multiple Choice)
4.9/5  (35)
(35)
A patient receiving continuous mandatory ventilation in the assist-control mode develops auto-PEEP. Which of the following changes in ventilatory patterns would you consider to minimize the effects of auto-PEEP in this patient?
1) Decreasing the rate or increasing VT
2) Using low-rate synchronized intermittent mandatory ventilation
3) Decreasing the peak inspiratory flow
4) Lowering the VT and letting the PaCO2 rise
(Multiple Choice)
4.9/5  (33)
(33)
Which of the following would decrease PaCO2 when ventilating a patient using intermittent mandatory ventilation with pressure support?
(Multiple Choice)
4.9/5  (39)
(39)
What is the predicted change in tidal volume by adding 6 in of tubing to a ventilator circuit?
(Multiple Choice)
4.8/5  (41)
(41)
When using a heated humidifier during mechanical ventilation, the inspired gas temperature at the airway should be set to what level?
(Multiple Choice)
4.8/5  (34)
(34)
In what clinical condition has pressure-controlled ventilation with a prolonged inspiratory time been shown to be helpful?
(Multiple Choice)
4.8/5  (41)
(41)
Which of the following criteria should be met before considering use of a heat-moisture exchanger (HME) for a patient being placed on ventilatory support?
1) There should be no problem with retained secretions.
2) The patient should not have fever (normothermic).
3) The patient should be adequately hydrated.
4) The support should be short term (24 to 48 hr).
(Multiple Choice)
4.7/5  (34)
(34)
Indications for delivering sigh breaths during mechanical ventilation include which of the following?
1) Before and after suctioning
2) During chest physical therapy
3) In patients with stiff lungs
4) When small VT values are used
(Multiple Choice)
4.8/5  (40)
(40)
On a ventilator that has separate rate and minute ventilation (VE) controls, the rate is set at 13/min and the VE at 11 L/min. Approximately what VT is the patient receiving?
(Multiple Choice)
4.8/5  (44)
(44)
What flow pattern is least optimal for ventilating a patient with cardiovascular instability?
(Multiple Choice)
4.8/5  (35)
(35)
In what scenario is pressure-controlled ventilation (PCV) most often used?
(Multiple Choice)
4.9/5  (37)
(37)
Which of the following would you initially verify in assessing the airway of a patient placed on ventilatory support?
1) Cuff pressure
2) Tube position
3) Tube patency
(Multiple Choice)
4.9/5  (40)
(40)
Compared to a pressure-controlled strategy, what is the primary advantage of volume-controlled ventilatory support?
(Multiple Choice)
4.9/5  (39)
(39)
For adolescents in the 8- to 16-year-old age range, which of the following ranges of ventilator setting would you initially recommend? Rate VT
(Multiple Choice)
4.9/5  (39)
(39)
The following data are gathered during a PEEP study (FiO2 = 0.60). Based on these data, what is the optimum PEEP level? 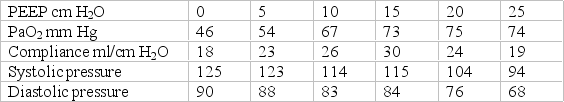
(Multiple Choice)
4.9/5  (38)
(38)
A heat-moisture exchanger (HME) should be avoided in which of the following circumstances?
1) Patients with excessive secretions
2) Patients with a high FiO2
3) Patients with low body temperature
(Multiple Choice)
4.9/5  (38)
(38)
Showing 21 - 40 of 97
Filters
- Essay(0)
- Multiple Choice(0)
- Short Answer(0)
- True False(0)
- Matching(0)