Deck 14: Sexually Transmitted Infections
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/70
Play
Full screen (f)
Deck 14: Sexually Transmitted Infections
1
The prevalence of syphilis fell dramatically during the 20th century, mainly because of
A) the use of condoms.
B) the use of antibiotics.
C) the near-elimination of prostitution.
D) public health advertising campaigns.
E) control of disease spread by the military.
A) the use of condoms.
B) the use of antibiotics.
C) the near-elimination of prostitution.
D) public health advertising campaigns.
E) control of disease spread by the military.
B
2
In comparing syphilis and AIDS, AIDS is currently considered
A) more serious because it cannot yet be cured.
B) more serious because it spreads more rapidly.
C) more serious because it is found on more continents.
D) less serious because it has been controlled much more quickly.
E) less serious because it can be controlled without antibiotics.
A) more serious because it cannot yet be cured.
B) more serious because it spreads more rapidly.
C) more serious because it is found on more continents.
D) less serious because it has been controlled much more quickly.
E) less serious because it can be controlled without antibiotics.
A
3
A review of the demographics of STIs in the United States reveals that
A) about one million people are diagnosed with STIs every year.
B) America has a higher incidence of STIs than other developed countries.
C) rates of all STIs are declining in the United States.
D) there are no regional differences in STI rates.
E) white Americans have lower rates of STIs than any other racial group.
A) about one million people are diagnosed with STIs every year.
B) America has a higher incidence of STIs than other developed countries.
C) rates of all STIs are declining in the United States.
D) there are no regional differences in STI rates.
E) white Americans have lower rates of STIs than any other racial group.
B
4
Refer to the table.
 Source: CDC. 2019. Sexually Transmitted Diseases Surveillance 2018; HHS.gov. 2019. Hepatitis B basic information; HIV.gov. 2019. U.S. statistics. U.S. Department of Health and Human Services: Washington, D.C. and Atlanta, GA; and other sources.
Source: CDC. 2019. Sexually Transmitted Diseases Surveillance 2018; HHS.gov. 2019. Hepatitis B basic information; HIV.gov. 2019. U.S. statistics. U.S. Department of Health and Human Services: Washington, D.C. and Atlanta, GA; and other sources.
aIn age range 15 to 49; total is higher.
bHepatitis B and HIV infections are not all by sexual contact.
Based on prevalence alone, which diseases would presently be considered the most common STIs in the United States?
A) Chlamydia and HIV
B) Trichomoniasis and chlamydia
C) Trichomoniasis and HPV
D) Genital herpes and HPV
E) Gonorrhea and genital herpes
 Source: CDC. 2019. Sexually Transmitted Diseases Surveillance 2018; HHS.gov. 2019. Hepatitis B basic information; HIV.gov. 2019. U.S. statistics. U.S. Department of Health and Human Services: Washington, D.C. and Atlanta, GA; and other sources.
Source: CDC. 2019. Sexually Transmitted Diseases Surveillance 2018; HHS.gov. 2019. Hepatitis B basic information; HIV.gov. 2019. U.S. statistics. U.S. Department of Health and Human Services: Washington, D.C. and Atlanta, GA; and other sources.aIn age range 15 to 49; total is higher.
bHepatitis B and HIV infections are not all by sexual contact.
Based on prevalence alone, which diseases would presently be considered the most common STIs in the United States?
A) Chlamydia and HIV
B) Trichomoniasis and chlamydia
C) Trichomoniasis and HPV
D) Genital herpes and HPV
E) Gonorrhea and genital herpes

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
5
A man has a sexual encounter during which his partner passes the AIDS virus to him. The virus becomes established in his body, but he remains asymptomatic. Does this man have an STI (sexually transmitted infection) or an STD (sexually transmitted disease)?
A) Neither; he is asymptomatic.
B) Both; an STI is the same as an STD.
C) An STI; he has an infection but no symptoms.
D) An STD; he has an infection that causes a disease.
E) An STD; he has an infection that can be transmitted.
A) Neither; he is asymptomatic.
B) Both; an STI is the same as an STD.
C) An STI; he has an infection but no symptoms.
D) An STD; he has an infection that causes a disease.
E) An STD; he has an infection that can be transmitted.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
6
A man with pubic lice uses an over-the-counter insecticide to remove them. He is fine for about a week, but then begins itching again. What is the most likely reason?
A) The insecticide only killed some of the lice.
B) The insecticide weakened the lice, but they recovered.
C) The treated lice fell off his body and survived in his bedding for a week.
D) The man encountered another person with lice and he got them again.
E) The insecticide killed the adult lice, but the nits survived and hatched.
A) The insecticide only killed some of the lice.
B) The insecticide weakened the lice, but they recovered.
C) The treated lice fell off his body and survived in his bedding for a week.
D) The man encountered another person with lice and he got them again.
E) The insecticide killed the adult lice, but the nits survived and hatched.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
7
The most common treatment for pubic lice (crabs) is
A) hot baths.
B) removal by hand.
C) over-the-counter insecticides.
D) antibiotic ointment.
E) waiting for the infestation to run its course.
A) hot baths.
B) removal by hand.
C) over-the-counter insecticides.
D) antibiotic ointment.
E) waiting for the infestation to run its course.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
8
It ordinarily takes two treatments of permethrin lotion to eradicate a scabies infection. The second treatment is necessary because
A) some surface mites survive the first treatment.
B) viable eggs may hatch after the first treatment.
C) mites are weakened by the first treatment and killed by the second.
D) deeply hidden adult mites come to the surface after the first treatment.
E) mites hidden in the pubic hairs may be missed and require a second treatment.
A) some surface mites survive the first treatment.
B) viable eggs may hatch after the first treatment.
C) mites are weakened by the first treatment and killed by the second.
D) deeply hidden adult mites come to the surface after the first treatment.
E) mites hidden in the pubic hairs may be missed and require a second treatment.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
9
Both members of a couple are diagnosed with the protozoan infection, trichomoniasis. Are they equally likely to show symptoms, or is the man or the woman more likely?
A) The man is more likely; about sixty percent of men show symptoms, compared to forty percent of women.
B) The man is more likely; about three-fourths of men show symptoms, while almost all women are asymptomatic.
C) The woman is more likely; about sixty percent of women show symptoms, compared to forty percent of men.
D) The woman is more likely; about three-fourths of women show symptoms, while almost all men are asymptomatic.
E) They are equally likely; gender has no bearing on whether they show symptoms.
A) The man is more likely; about sixty percent of men show symptoms, compared to forty percent of women.
B) The man is more likely; about three-fourths of men show symptoms, while almost all women are asymptomatic.
C) The woman is more likely; about sixty percent of women show symptoms, compared to forty percent of men.
D) The woman is more likely; about three-fourths of women show symptoms, while almost all men are asymptomatic.
E) They are equally likely; gender has no bearing on whether they show symptoms.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
10
One member of a couple is diagnosed with trichomoniasis and treated. Should the other person be treated as well, and if so, why?
A) Yes, if both are treated, the infected partner will be cured more rapidly.
B) Yes, if both are not treated, they will keep passing the infection back and forth.
C) No, if the other person is not infected, there is no reason to treat him or her.
D) No, treating both is only necessary if the infected person has an extremely serious case.
E) It doesn't matter; if one is treated, they will both be cured.
A) Yes, if both are treated, the infected partner will be cured more rapidly.
B) Yes, if both are not treated, they will keep passing the infection back and forth.
C) No, if the other person is not infected, there is no reason to treat him or her.
D) No, treating both is only necessary if the infected person has an extremely serious case.
E) It doesn't matter; if one is treated, they will both be cured.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
11
A trichomoniasis infection is caused by which type of organism?
A) Mite
B) Virus
C) Louse
D) Protozoan
E) Bacterium
A) Mite
B) Virus
C) Louse
D) Protozoan
E) Bacterium

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
12
A woman notices a foul-smelling greenish discharge from her vagina, while her husband has no symptoms. Both may be infected with which sexually transmitted infection?
A) Scabies
B) Syphilis
C) Gonorrhea
D) Genital herpes
E) Trichomoniasis
A) Scabies
B) Syphilis
C) Gonorrhea
D) Genital herpes
E) Trichomoniasis

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
13
Which STI can be successfully treated with antibiotics?
A) HIV
B) Scabies
C) Syphilis
D) Pubic lice
E) Hepatitis A
A) HIV
B) Scabies
C) Syphilis
D) Pubic lice
E) Hepatitis A

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
14
During which stage or stages of untreated syphilis can the disease be passed to sex partners?
A) Primary phase only
B) Secondary phase only
C) Early latent phase only
D) Secondary and early latent phases only
E) Primary, secondary, and early latent phases
A) Primary phase only
B) Secondary phase only
C) Early latent phase only
D) Secondary and early latent phases only
E) Primary, secondary, and early latent phases

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
15
A gay man has a painless, reddish rash covering the palms of his hands. He reports having an open sore on his penis several months earlier, but he did not seek treatment because the sore went away. Based on these symptoms, the man most likely has
A) AIDS, because it is common in gay men.
B) scabies, because of the sore on his penis.
C) primary syphilis, because of the sore on his penis.
D) secondary syphilis, because of the sore followed by the rash.
E) HPV, because HPV is the most common STI in the United States.
A) AIDS, because it is common in gay men.
B) scabies, because of the sore on his penis.
C) primary syphilis, because of the sore on his penis.
D) secondary syphilis, because of the sore followed by the rash.
E) HPV, because HPV is the most common STI in the United States.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
16
A previously healthy man is diagnosed with both secondary syphilis and HIV. What is the most likely way he contracted HIV?
A) He had unprotected sex with one partner who had contracted syphilis 18 months before their encounter and was also HIV positive; HIV and syphilis are usually transferred together.
B) He had unprotected sex with an HIV positive partner while he had open chancres from primary syphilis, which increased his risk for contracting HIV.
C) He had protected sex with an HIV positive partner while his syphilis was in its second year of latency.
D) He must have recently had unprotected sex with two differently infected partners; HIV and syphilis must be transferred independently, from different sexual partners.
E) The syphilis spirochete attacked his immune system, making it easier for him to contract HIV from nonsexual contact.
A) He had unprotected sex with one partner who had contracted syphilis 18 months before their encounter and was also HIV positive; HIV and syphilis are usually transferred together.
B) He had unprotected sex with an HIV positive partner while he had open chancres from primary syphilis, which increased his risk for contracting HIV.
C) He had protected sex with an HIV positive partner while his syphilis was in its second year of latency.
D) He must have recently had unprotected sex with two differently infected partners; HIV and syphilis must be transferred independently, from different sexual partners.
E) The syphilis spirochete attacked his immune system, making it easier for him to contract HIV from nonsexual contact.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
17
Which observation would provide the most definitive diagnosis of syphilis?
A) Observation of chancres
B) A fever and a rash on hands and feet
C) Observation of discharge from the penis or vagina
D) Detection of antibodies to Treponema pallidum in the blood
E) Knowledge that the person in question had sex with an infected partner
A) Observation of chancres
B) A fever and a rash on hands and feet
C) Observation of discharge from the penis or vagina
D) Detection of antibodies to Treponema pallidum in the blood
E) Knowledge that the person in question had sex with an infected partner

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
18
Which statement most accurately describes the status of syphilis in the United States today?
A) It has been almost completely eliminated by antibiotic treatment.
B) There is a lower incidence today than a century ago, but a large percentage of cases still progress to the tertiary phase.
C) It has recently rebounded, with three distinct, interconnected epidemics.
D) It has recently rebounded, with a clear epidemic across all sexually active populations.
E) It is currently at low levels, but new mutations have significantly increased infection rates.
A) It has been almost completely eliminated by antibiotic treatment.
B) There is a lower incidence today than a century ago, but a large percentage of cases still progress to the tertiary phase.
C) It has recently rebounded, with three distinct, interconnected epidemics.
D) It has recently rebounded, with a clear epidemic across all sexually active populations.
E) It is currently at low levels, but new mutations have significantly increased infection rates.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
19
All of the following were ethical problems with the Tuskegee syphilis study except that participants
A) did not give informed consent.
B) were denied standard care for syphilis.
C) were deliberately infected with syphilis.
D) falsely believed they were being treated for syphilis.
E) were allowed to infect others and die.
A) did not give informed consent.
B) were denied standard care for syphilis.
C) were deliberately infected with syphilis.
D) falsely believed they were being treated for syphilis.
E) were allowed to infect others and die.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
20
Mark has sex with a woman he just met. A few days later, he begins to experience a burning sensation during urination, followed by yellow discharge from his urethra. It is likely that Mark has contracted
A) herpes.
B) syphilis.
C) molluscum contagiosum.
D) gonorrhea.
E) genital warts.
A) herpes.
B) syphilis.
C) molluscum contagiosum.
D) gonorrhea.
E) genital warts.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
21
One year ago, a pregnant 22-year-old had a chlamydia infection that was treated successfully. She currently has no symptoms of gonorrhea, but she has had several sexual encounters without condoms. Would a doctor likely consider her baby at risk for gonorrhea?
A) No; she had chlamydia, not gonorrhea.
B) No; she has no symptoms of gonorrhea.
C) No; gonorrhea is rarely transmitted during childbirth.
D) Definitely; her history of multiple sexual partners makes gonorrhea very likely.
E) Possibly; gonorrhea is often asymptomatic and can be easily transmitted during childbirth.
A) No; she had chlamydia, not gonorrhea.
B) No; she has no symptoms of gonorrhea.
C) No; gonorrhea is rarely transmitted during childbirth.
D) Definitely; her history of multiple sexual partners makes gonorrhea very likely.
E) Possibly; gonorrhea is often asymptomatic and can be easily transmitted during childbirth.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
22
Because the gonorrhea bacterium has become increasingly drug resistant, the CDC now recommends
A) no treatment; the infection will run its course.
B) larger-than-normal doses of a common antibiotic, such as penicillin.
C) larger-than-normal doses of penicillin plus antiviral drugs.
D) a combination of injected and oral antibiotics.
E) the same cocktail of antiviral medication as is used to treat HIV.
A) no treatment; the infection will run its course.
B) larger-than-normal doses of a common antibiotic, such as penicillin.
C) larger-than-normal doses of penicillin plus antiviral drugs.
D) a combination of injected and oral antibiotics.
E) the same cocktail of antiviral medication as is used to treat HIV.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
23
A young woman contracted a gonorrheal infection that was successfully treated with antibiotics. In considering the likelihood of future gonorrheal infections, she should
A) always be careful; reinfection can occur at any time.
B) wait to have sex until after a vaccine against gonorrhea is available.
C) not worry; having had the disease, she now is immune for life.
D) notify all future partners because she is a lifelong carrier.
E) avoid having sex for the next few months until she builds up antibodies.
A) always be careful; reinfection can occur at any time.
B) wait to have sex until after a vaccine against gonorrhea is available.
C) not worry; having had the disease, she now is immune for life.
D) notify all future partners because she is a lifelong carrier.
E) avoid having sex for the next few months until she builds up antibodies.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
24
Which two sexually transmitted infections may escalate into pelvic inflammatory disease (PID) if untreated?
A) Syphilis and herpes
B) Chlamydia and herpes
C) Chlamydia and gonorrhea
D) Trichomoniasis and gonorrhea
E) Trichomoniasis and bacterial vaginosis
A) Syphilis and herpes
B) Chlamydia and herpes
C) Chlamydia and gonorrhea
D) Trichomoniasis and gonorrhea
E) Trichomoniasis and bacterial vaginosis

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
25
A student learns that the organism causing syphilis, T. pallidum, is easily treated and killed using penicillin. He assumes this will also be true for N. gonorrhoeae, the organism that causes gonorrhea since it is also a bacterium. Is he correct?
A) Yes, any bacterial STI can be treated with antibiotics such as penicillin.
B) Yes, the organisms causing both syphilis and gonorrhea can be killed with penicillin.
C) No, gonorrhea is resistant to penicillin but can be treated with most other antibiotics.
D) No, gonorrhea has developed drug resistance to several different classes of antibiotics, including penicillin.
E) No, gonorrhea cannot be treated with penicillin or other antibiotics because it is not caused by a bacterium.
A) Yes, any bacterial STI can be treated with antibiotics such as penicillin.
B) Yes, the organisms causing both syphilis and gonorrhea can be killed with penicillin.
C) No, gonorrhea is resistant to penicillin but can be treated with most other antibiotics.
D) No, gonorrhea has developed drug resistance to several different classes of antibiotics, including penicillin.
E) No, gonorrhea cannot be treated with penicillin or other antibiotics because it is not caused by a bacterium.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
26
How do chlamydia infections in tropical countries differ from those in the United States?
A) They are caused by a different organism.
B) Their symptoms are more localized.
C) They are often transmitted by insects.
D) They occur more frequently in women than in men.
E) They are most common in young, sexually active men and women.
A) They are caused by a different organism.
B) Their symptoms are more localized.
C) They are often transmitted by insects.
D) They occur more frequently in women than in men.
E) They are most common in young, sexually active men and women.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
27
Jennifer develops painful urination and slight, watery vaginal discharge two weeks after her first coital encounter with her new boyfriend, who shows no symptoms of any STIs. She does not see her doctor, and later comes down with a fever and severe abdominal cramps. At this point, she visits a doctor who diagnoses her with PID. Jennifer's PID most likely was caused by an untreated case of
A) syphilis.
B) HPV.
C) chlamydia.
D) genital herpes.
E) trichomoniasis.
A) syphilis.
B) HPV.
C) chlamydia.
D) genital herpes.
E) trichomoniasis.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
28
What is the CDC's general recommendation for testing women for chlamydia?
A) All women should be tested once per year.
B) All women should be tested once every five years.
C) All sexually active women should be tested once per year.
D) All women should be tested once per year if they are under 25, pregnant, or have a new sex partner.
E) Women should be tested for chlamydia only if they show symptoms.
A) All women should be tested once per year.
B) All women should be tested once every five years.
C) All sexually active women should be tested once per year.
D) All women should be tested once per year if they are under 25, pregnant, or have a new sex partner.
E) Women should be tested for chlamydia only if they show symptoms.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
29
Since 1985, there have been many more reported cases of genital chlamydia in the United States. Doctors think this increase is most likely due to
A) a new epidemic, similar to AIDS in the 1980s.
B) mutation to a more virulent strain.
C) increased recognition and diagnosis of an existing condition.
D) a significant increase in unprotected sex among young people.
E) a recent flare-up of cases that had been latent for several decades.
A) a new epidemic, similar to AIDS in the 1980s.
B) mutation to a more virulent strain.
C) increased recognition and diagnosis of an existing condition.
D) a significant increase in unprotected sex among young people.
E) a recent flare-up of cases that had been latent for several decades.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
30
A doctor is most likely to suspect bacterial vaginosis if a woman experiences
A) open sores on her vulva.
B) a fishy-smelling discharge.
C) a thick yellowish discharge.
D) a highly acidic vaginal pH.
E) a higher-than-normal count of lactobacilli.
A) open sores on her vulva.
B) a fishy-smelling discharge.
C) a thick yellowish discharge.
D) a highly acidic vaginal pH.
E) a higher-than-normal count of lactobacilli.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
31
The female of a heterosexual couple is diagnosed with bacterial vaginosis but has shown no symptoms. Should she be treated and if so, why?
A) No, treatment is unnecessary since she has no symptoms.
B) No, treatment is unnecessary since it will go away on its own.
C) No, she has no symptoms and her partner cannot contract a vaginal infection.
D) Yes, but only if she is pregnant; it can cause premature birth and low birth weight.
E) Yes, it may cause PID and make it easier to acquire other STDs.
A) No, treatment is unnecessary since she has no symptoms.
B) No, treatment is unnecessary since it will go away on its own.
C) No, she has no symptoms and her partner cannot contract a vaginal infection.
D) Yes, but only if she is pregnant; it can cause premature birth and low birth weight.
E) Yes, it may cause PID and make it easier to acquire other STDs.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
32
A woman develops an inflammation of the urethra, which spreads to her reproductive tract. She is treated with antibiotics but the treatment is unsuccessful. She is most likely suffering from
A) nongonococcal urethritis caused by the bacterium Mycoplasma genitalium.
B) nongonococcal urethritis caused by Gardnerella vaginalis.
C) chlamydia.
D) bacterial vaginosis.
E) syphilis.
A) nongonococcal urethritis caused by the bacterium Mycoplasma genitalium.
B) nongonococcal urethritis caused by Gardnerella vaginalis.
C) chlamydia.
D) bacterial vaginosis.
E) syphilis.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
33
A short-lived Zika virus epidemic occurred in Brazil in 2014, followed by a smaller outbreak in the United States in 2016. The history of the Zika virus supports which conclusion about viral STIs?
A) Newly emerging viruses will likely be less dangerous than earlier viruses, such as HIV.
B) Viruses are either sexually transmitted or not; they cannot be transmitted in multiple ways.
C) Sexually transmitted viruses, such as Zika, are not dangerous and can usually be ignored.
D) New, potentially dangerous viruses can emerge at any time and may be transmitted in more than one way.
E) Zika-type viruses are only a danger in tropical areas, such as Brazil, not in the United States.
A) Newly emerging viruses will likely be less dangerous than earlier viruses, such as HIV.
B) Viruses are either sexually transmitted or not; they cannot be transmitted in multiple ways.
C) Sexually transmitted viruses, such as Zika, are not dangerous and can usually be ignored.
D) New, potentially dangerous viruses can emerge at any time and may be transmitted in more than one way.
E) Zika-type viruses are only a danger in tropical areas, such as Brazil, not in the United States.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
34
A man sees his doctor about bumps on his skin. The doctor tells him they are caused by a highly contagious virus, and they will disappear without treatment within a year, but the bumps can be removed now by freezing them. The man is most likely infected with a
A) pox virus.
B) hepatitis virus.
C) herpes simplex virus.
D) human papillomavirus.
E) human immunodeficiency virus.
A) pox virus.
B) hepatitis virus.
C) herpes simplex virus.
D) human papillomavirus.
E) human immunodeficiency virus.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
35
The main difference between herpes simplex 1 (HSV-1) and herpes simplex 2 (HSV-2) is
A) they are caused by different herpes viruses.
B) HSV-2 can be sexually transmitted; HSV-1 cannot.
C) HSV-1 can be cured; HSV-2 cannot.
D) HSV-1 affects only the mouth; HSV-2 affects only the genitals.
E) HSV-1 affects only the genitals; HSV-2 affects only the mouth.
A) they are caused by different herpes viruses.
B) HSV-2 can be sexually transmitted; HSV-1 cannot.
C) HSV-1 can be cured; HSV-2 cannot.
D) HSV-1 affects only the mouth; HSV-2 affects only the genitals.
E) HSV-1 affects only the genitals; HSV-2 affects only the mouth.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
36
A man has sores on his penis that are diagnosed as HSV-1. He was most likely infected as a result of
A) oral sex.
B) anal sex with a heterosexual partner.
C) anal sex with a homosexual partner.
D) heterosexual coitus.
E) masturbation.
A) oral sex.
B) anal sex with a heterosexual partner.
C) anal sex with a homosexual partner.
D) heterosexual coitus.
E) masturbation.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
37
A woman has had intermittent and severe recurrences of herpes over the past three years. Her doctor prescribes the antiviral drug acyclovir, to be taken continually as a preventive measure. Does this woman most likely have HSV-1 or HSV-2?
A) HSV-1, because acyclovir works only on HSV-1
B) HSV-2, because acyclovir works only on HSV-2
C) HSV-1, because the recurrences have lasted three years
D) HSV-2, because the recurrences have lasted three years
E) Either, as both are equally serious and long-lasting
A) HSV-1, because acyclovir works only on HSV-1
B) HSV-2, because acyclovir works only on HSV-2
C) HSV-1, because the recurrences have lasted three years
D) HSV-2, because the recurrences have lasted three years
E) Either, as both are equally serious and long-lasting

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
38
An outbreak of genital herpes (HSV-2) on the penis or labia is indicated by symptoms that follow a predictable course: itching, followed by clusters of spots that form blisters, and then open sores. At which phase in the outbreak is the virus most contagious?
A) Before itching begins
B) When there is itching
C) When there are spots
D) When there are blisters
E) When there are open sores
A) Before itching begins
B) When there is itching
C) When there are spots
D) When there are blisters
E) When there are open sores

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
39
After an initial outbreak of genital herpes, the viral particles travel to the nerve cell bodies along the spinal cord. At this time, the viral particles are
A) unable to leave the nerve cells.
B) unable to reproduce in the nerve cells.
C) protected from the body's immune system.
D) likely to spread throughout the host's body.
E) likely to generate a new, more virulent infection.
A) unable to leave the nerve cells.
B) unable to reproduce in the nerve cells.
C) protected from the body's immune system.
D) likely to spread throughout the host's body.
E) likely to generate a new, more virulent infection.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
40
Jeff has never had a recognized outbreak of HSV-2, but viral antibodies are present in his blood. What is the most important implication of his situation?
A) It shows he has a very strong immune system.
B) It shows he was once exposed to HSV-2 but never became infected.
C) It shows he was once infected but was never contagious.
D) It means he is a carrier and can transmit the virus to sex partners during outbreaks.
E) It suggests the virus is building up and may cause a serious infection later.
A) It shows he has a very strong immune system.
B) It shows he was once exposed to HSV-2 but never became infected.
C) It shows he was once infected but was never contagious.
D) It means he is a carrier and can transmit the virus to sex partners during outbreaks.
E) It suggests the virus is building up and may cause a serious infection later.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
41
Babies are at risk of getting a herpes infection from their mothers during childbirth, sometimes with fatal consequences. Given that a person exposed to herpes will develop antibodies to the disease, a mother who is most likely to pass the virus to her child is one
A) who has not had herpes in several years.
B) who had herpes just before getting pregnant.
C) who had herpes early in pregnancy.
D) who had herpes very late in pregnancy.
E) whose baby is delivered by caesarian section.
A) who has not had herpes in several years.
B) who had herpes just before getting pregnant.
C) who had herpes early in pregnancy.
D) who had herpes very late in pregnancy.
E) whose baby is delivered by caesarian section.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
42
A woman develops a series of small bumps or warts around the opening to her vagina. They are painless, but soon afterward, her boyfriend develops similar warts on his penis. It is likely that this couple is infected by
A) genital warts caused by HPV type 6 or 11.
B) genital warts caused by HPV type 16 or 18.
C) precancerous lesions caused by any type of HPV.
D) precancerous lesions caused by herpes virus HSV-2.
E) non-cancerous lesions caused by herpes virus HSV-2.
A) genital warts caused by HPV type 6 or 11.
B) genital warts caused by HPV type 16 or 18.
C) precancerous lesions caused by any type of HPV.
D) precancerous lesions caused by herpes virus HSV-2.
E) non-cancerous lesions caused by herpes virus HSV-2.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
43
A doctor would most likely use a Pap test to determine if a person has
A) oral cancer.
B) penile cancer.
C) a genital HPV infection.
D) warts around the genitals.
E) warning signs of cervical cancer.
A) oral cancer.
B) penile cancer.
C) a genital HPV infection.
D) warts around the genitals.
E) warning signs of cervical cancer.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
44
HPV vaccination may have a more dramatic effect on people's health in the developing world than in the United States because
A) most American youths are already vaccinated and therefore not at risk.
B) HPV has been nearly eliminated in the United States.
C) people in developing countries seldom have access to Pap tests.
D) HPV strains in other parts of the world are more virulent than strains in the United States.
E) people in developing countries are more likely than U.S. citizens to be exposed to HPV.
A) most American youths are already vaccinated and therefore not at risk.
B) HPV has been nearly eliminated in the United States.
C) people in developing countries seldom have access to Pap tests.
D) HPV strains in other parts of the world are more virulent than strains in the United States.
E) people in developing countries are more likely than U.S. citizens to be exposed to HPV.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
45
There are approximately 100 kinds of human papillomaviruses (HPV). Two of these, HPV 16 and 18, are responsible for
A) most cases of genital warts.
B) most cases of cervical cancer.
C) most cancers of the mouth and throat.
D) common skin warts, but not genital warts.
E) all cases of genital warts that eventually become cancer.
A) most cases of genital warts.
B) most cases of cervical cancer.
C) most cancers of the mouth and throat.
D) common skin warts, but not genital warts.
E) all cases of genital warts that eventually become cancer.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
46
A young gay man is diagnosed with the hepatitis A virus. He most likely picked up the virus through
A) fecal-oral transmission.
B) nonsexual transmission.
C) anal sex with an infected partner.
D) oral sex with an infected partner.
E) contact with contaminated blood.
A) fecal-oral transmission.
B) nonsexual transmission.
C) anal sex with an infected partner.
D) oral sex with an infected partner.
E) contact with contaminated blood.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
47
Dave has recently been diagnosed with hepatitis B. Given current knowledge and statistics related to this disease, Dave's most likely prognosis is that he will
A) recover and become noninfectious.
B) quickly overcome symptoms but remain permanently contagious.
C) develop serious liver damage within the first weeks of infection.
D) develop a chronic illness, but an extended treatment period will eliminate the virus.
E) develop a chronic illness, likely leading to liver cancer.
A) recover and become noninfectious.
B) quickly overcome symptoms but remain permanently contagious.
C) develop serious liver damage within the first weeks of infection.
D) develop a chronic illness, but an extended treatment period will eliminate the virus.
E) develop a chronic illness, likely leading to liver cancer.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
48
Which statement comparing hepatitis A and hepatitis B is correct?
A) There is a vaccine for hepatitis B, but not for hepatitis A.
B) There is a treatment for hepatitis A, but not for hepatitis B.
C) Hepatitis B usually has milder symptoms than hepatitis A.
D) Hepatitis B is often spread by food handlers, while hepatitis A is not.
E) Hepatitis A does not develop into a chronic disease, while hepatitis B can.
A) There is a vaccine for hepatitis B, but not for hepatitis A.
B) There is a treatment for hepatitis A, but not for hepatitis B.
C) Hepatitis B usually has milder symptoms than hepatitis A.
D) Hepatitis B is often spread by food handlers, while hepatitis A is not.
E) Hepatitis A does not develop into a chronic disease, while hepatitis B can.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
49
A couple is engaging in unprotected sex. The risk of a member of the couple contracting an HIV infection is greatest for
A) the male during vaginal sex.
B) the female during vaginal sex.
C) the male during anal sex.
D) the female during anal sex.
E) the male during oral sex.
A) the male during vaginal sex.
B) the female during vaginal sex.
C) the male during anal sex.
D) the female during anal sex.
E) the male during oral sex.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
50
A major result of the process of seroconversion during infection with HIV is that a person
A) becomes temporarily unable to transmit the disease.
B) shows a drop in CD4 levels to 200 µL or less.
C) experiences an opportunistic illness, such as pneumonia.
D) produces antibodies to HIV, and blood levels of HIV decrease.
E) produces antibodies to HIV, and the body eliminates the disease.
A) becomes temporarily unable to transmit the disease.
B) shows a drop in CD4 levels to 200 µL or less.
C) experiences an opportunistic illness, such as pneumonia.
D) produces antibodies to HIV, and blood levels of HIV decrease.
E) produces antibodies to HIV, and the body eliminates the disease.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
51
Given that the body is able to produce antibodies against HIV, why do many people still progress from HIV infection to full-blown AIDS?
A) HIV attacks cells in the immune system, compromising the body's ability to make and use antibodies.
B) HIV reproduces too rapidly for the immune system to cope, even though it is working at full capacity.
C) Many other diseases are associated with AIDS, and the immune system uses its HIV antibodies to fight these diseases.
D) Infected people usually delay getting diagnosed, and by that time it is too late for antibodies to overcome the disease.
E) Many infected people are alcoholics and drug addicts who do not take care of themselves.
A) HIV attacks cells in the immune system, compromising the body's ability to make and use antibodies.
B) HIV reproduces too rapidly for the immune system to cope, even though it is working at full capacity.
C) Many other diseases are associated with AIDS, and the immune system uses its HIV antibodies to fight these diseases.
D) Infected people usually delay getting diagnosed, and by that time it is too late for antibodies to overcome the disease.
E) Many infected people are alcoholics and drug addicts who do not take care of themselves.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
52
Refer to the figure.
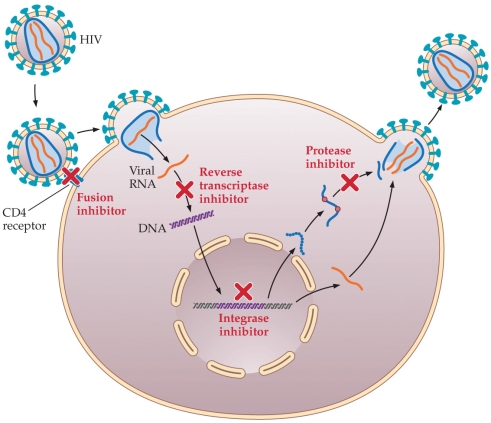 The figure illustrates the sites of actions of various antiretroviral drugs used to treat HIV and AIDS. The fusion inhibitor, or entry inhibitor, acts at which point in the HIV replication cycle?
The figure illustrates the sites of actions of various antiretroviral drugs used to treat HIV and AIDS. The fusion inhibitor, or entry inhibitor, acts at which point in the HIV replication cycle?
A) Before the virus enters the cell
B) Just as the virus enters the cell
C) Before the viral RNA is copied to DNA
D) Before the viral DNA is inserted into the host cell
E) Before new viral proteins are cut into short, functional lengths
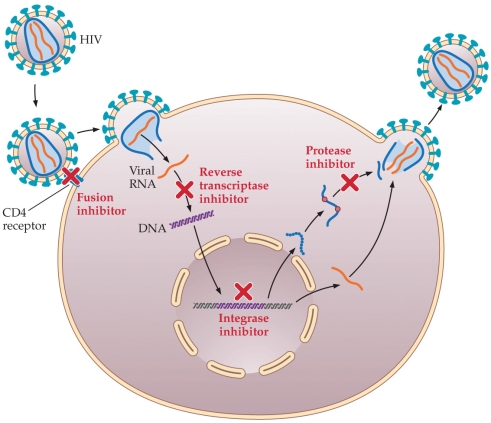 The figure illustrates the sites of actions of various antiretroviral drugs used to treat HIV and AIDS. The fusion inhibitor, or entry inhibitor, acts at which point in the HIV replication cycle?
The figure illustrates the sites of actions of various antiretroviral drugs used to treat HIV and AIDS. The fusion inhibitor, or entry inhibitor, acts at which point in the HIV replication cycle?A) Before the virus enters the cell
B) Just as the virus enters the cell
C) Before the viral RNA is copied to DNA
D) Before the viral DNA is inserted into the host cell
E) Before new viral proteins are cut into short, functional lengths

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
53
The worldwide AIDS pandemic shows some signs of abating, according to statistics collected between 2000 and 2016. This decline is most likely due to
A) new, highly effective antiviral drugs.
B) a new, highly effective AIDS vaccine.
C) the disease running its course and no new cases occurring.
D) the virus mutating into a less virulent and less infectious form.
E) people changing their behaviors so that infection is less likely.
A) new, highly effective antiviral drugs.
B) a new, highly effective AIDS vaccine.
C) the disease running its course and no new cases occurring.
D) the virus mutating into a less virulent and less infectious form.
E) people changing their behaviors so that infection is less likely.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
54
John is a sexually active gay man who has tested HIV-negative. What type of HIV treatment would his doctor most likely recommend for John?
A) No treatment
B) HIV vaccine
C) Post-exposure prophylaxis (PEP)
D) Pre-exposure prophylaxis (PrEP)
E) Antiviral drugs if CD4 levels drop below 200 µL
A) No treatment
B) HIV vaccine
C) Post-exposure prophylaxis (PEP)
D) Pre-exposure prophylaxis (PrEP)
E) Antiviral drugs if CD4 levels drop below 200 µL

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
55
AIDS was first recognized as a new disease when it
A) transferred from chimpanzees to humans.
B) caused outbreaks in African villages in the 1920s.
C) spread to countries in Europe and North America.
D) caused outbreaks in gay men in U.S. cities in the late 1970s.
E) caused infections in heterosexual men in Africa.
A) transferred from chimpanzees to humans.
B) caused outbreaks in African villages in the 1920s.
C) spread to countries in Europe and North America.
D) caused outbreaks in gay men in U.S. cities in the late 1970s.
E) caused infections in heterosexual men in Africa.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
56
Which behavior is most likely to prevent a person from contracting an STI?
A) Abstinence
B) Abstaining from anal sex
C) Always using a condom
D) Having only one sex partner
E) Not using intravenous drugs
A) Abstinence
B) Abstaining from anal sex
C) Always using a condom
D) Having only one sex partner
E) Not using intravenous drugs

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
57
Which sexual behaviors carry the highest risk for STI transmission?
A) Coitus and oral sex
B) Fellatio and cunnilingus
C) Coitus and hand-genital contact
D) Anal sex and coitus
E) Anilingus and fellatio
A) Coitus and oral sex
B) Fellatio and cunnilingus
C) Coitus and hand-genital contact
D) Anal sex and coitus
E) Anilingus and fellatio

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
58
Which condition is not an STI but is sometimes mistaken for herpes?
A) Folliculitis
B) Labial cysts
C) Canker sores
D) Genital warts
E) Pearly penile papules
A) Folliculitis
B) Labial cysts
C) Canker sores
D) Genital warts
E) Pearly penile papules

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
59
Discuss the history of STIs, including transmission, prevalence, early views of STIs, the beliefs about the morality of those infected, and the resulting individual, social, and political responses to STIs.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
60
Provide evidence to support the claim that STIs are still a major problem in the United States.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
61
Compare and contrast two STIs caused by insects or mites. Describe how each is treated.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
62
Discuss the progression of untreated syphilis and the way it is treated.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
63
Explain the similarities and differences between gonorrhea and chlamydia infections and their treatments.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
64
Design a brochure intended for college students describing the signs, symptoms, and treatment of chlamydia.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
65
Explain the similarities and differences between oral herpes and genital herpes, and discuss the possible effects of each on a sexual relationship.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
66
Discuss the cause, appearance, symptoms, progression, treatment, and consequences of genital warts.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
67
Explain the relationship between human papillomaviruses and cancer.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
68
Discuss the sexual transmission, signs, symptoms, and methods of prevention for both hepatitis A and hepatitis B.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
69
Discuss the many ways that HIV can be transmitted from an infected person to a non-infected person.

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck
70
You have been hired to design a public health campaign to alter behavior and reduce STI prevalence among young Americans. What will you include in your campaign, and how will you get the message across to the public?

Unlock Deck
Unlock for access to all 70 flashcards in this deck.
Unlock Deck
k this deck


