Multiple Choice
An intubated patient with chronic obstructive pulmonary disease (COPD) is breathing on pressure support ventilation (PSV) 13 cm H₂O with positive end-expiratory pressure (PEEP) 5 cm H₂O and a flow cycle setting of 25%.The pressure-time scalar shown in the figure is evaluated by the respiratory therapist.What action should the respiratory therapist take at this time?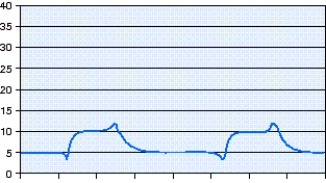
A) The patient and ventilator are synchronized and no change should be made.
B) The inspiratory flow rate should be increased to match the patient's needs.
C) The flow cycle setting should be increased to allow more time for exhalation.
D) The pressure support setting should be increased to match the peak pressure.
Correct Answer:

Verified
Correct Answer:
Verified
Q5: What is the flow rate necessary to
Q6: A 57-year-old,5'3",165 lb female patient arrives in
Q7: A 63-year-old,5'11",185 lb male patient with a
Q8: With which flow waveform pattern will the
Q9: A 5'10" male patient with normal lungs
Q11: A patient having an acute,severe asthma exacerbation
Q12: A 47-year-old,6'1" male patient is admitted to
Q13: A patient receiving mechanical ventilation via pressure-regulated
Q14: A 65-year-old,73-inch-tall,195 lb male patient was admitted
Q15: A 39-year-old,5'4",138 lb female patient requires intubation