Essay
AUDIT REPORT T1.2 OBSERVATION
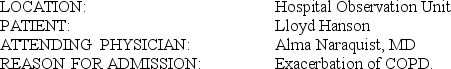 HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.
HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old male who comes in tonight complaining of progressive shortness of breath over the past 4 days. He had upper-respiratory tract symptoms a week ago with nasal discharge and cold-like symptoms. It progressed to shortness of breath over the past 4 days. I was called by a family member of his earlier tonight, and I advised him to come to the Emergency Room, which he did. In the ER, he was wheezy and had oxygen saturation of 92%. He received a nebulizer treatment. A chest x-ray was done, which I reviewed myself and showed no evidence of infiltrates. He has a large heart. The patient was admitted to the 6th floor.
I proceeded by doing ABGs on him. His pH was 7.46, PCO2 94, bicarb 33.5 on 2 liters per nasal cannula.
The patient has some cough with clear phlegm. No fever or chills now. He had some chills a week ago.
The patient recently had an angiogram for his abdominal aortic aneurysm.He also had a stress test that apparently was positive.
The patient is known to have chronic renal failure with a baseline creatinine of 2 to 2.2 with creatinine clearance of 32 ml per minute with a serum creatinine of 2.0 back in December.
He does have severe congestive heart failure with ejection fraction less than 20%.
PAST MEDICAL HISTORY:
1. Chronic renal failure as mentioned.
2. Coronary artery disease, post two myocardial infarctions.
3. Post AICD placement.
4. Atrial fibrillation with rapid ventricular response, controlled.
5. Congestive heart failure with ejection fraction of less than 20%.
6. Abdominal aortic aneurysm, which is infrarenal measuring 6.2 cm.
7. Bilateral common iliac aneurysm, approximately 3.5 to 3.6 cm.
8. Left internal iliac artery aneurysm, questionably coiled lately.
9. COPD/asthma.
10. History of gouty arthritis with a recent gouty attack in his right first metatarsal phalangeal joint.
11. History of diverticulitis.
12. Hyperlipidemia.
13. Status post cholecystectomy, inguinal hernia repair, appendectomy.
14. Chronic renal failure, post PD catheter placement.
ALLERGIES: No known drug allergies.
MEDICATIONS:
1. Nebulizer at home.
2. Bumex 2 mg in the morning and 1 mg in the evening.
3. Coumadin 2 mg on Monday, 1 mg on other days.
4. Digoxin 0.125 mg po daily.
5. Potassium chloride 20 mEq po b.i.d.
6. Zocor 10 mg po q.hs.
7. Coreg 25 mg po b.i.d.
8. Allopurinol 100 mg po daily.
9. Ranitidine 150 mg po q.hs.
FAMILY HISTORY: Mother died of pancreatitis. Father died at age 71. Otherwise, family history is noncontributory.
SOCIAL HISTORY: Lives here in town with his wife. She was not available today. He quit smoking 16 years ago.
REVIEW OF SYSTEMS: CONSTITUTIONAL: No fever, chills, or night sweats.
ENT: Resolved upper-respiratory tract symptoms. RESPIRATORY: As mentioned.
CARDIOVASCULAR: Exertional dyspnea. No chest pain. GI: Questionable dark stool but no diarrhea, nausea, or vomiting. He had some abdominal discomfort with coughing. MUSCULOSKELETAL: History of gouty arthritis, but seems to be controlled. SKIN: Trace edema. NEURO: Negative. PSYCHIATRIC: Negative.
PHYSICAL EXAMINATION: The patient was in mild respiratory distress. He was awake, oriented times three without any focal neurological deficits. His heart rate is in the 70s range, blood pressure has been 120s/80s, sats 92% when he came in, 98% on 2 liters per nasal cannula. Slightly increased jugular venous pressure. No cervical lymphadenopathy. LUNGS: Good air entry bilaterally but expiratory wheezes bilaterally. No crackles. No sacral edema. ABDOMEN: Soft and nontender, no masses. He has PD catheter in the left lower quadrant. Small hematoma in the right inguinal area from his recent aortogram.
LOWER EXTREMITIES: Very trace edema.
LABORATORY STUDIES: CBC tonight shows a white count of 8.6 thousand, hemoglobin 12.3, platelets 140,000, BUN 29, sodium 139, potassium 3.6, chloride 98, bicarb 31, creatinine 2.2, calcium 8.5. BNP 536 picogram/ml. INR 1.5 with a pro-time of 14.3. Digoxin 0.6. Troponin-I less than 0.04. His last uric acid level was 7.4.
IMPRESSION:
1. Exacerbation of COPD/asthma with wheezes.
2. Abdominal aortic aneurysm.
PLAN:
1. Albuterol MDI 2 puffs t.i.d.
2. Atrovent MDI 2 puffs t.i.d.
3. Azmacort MDI 2 puffs b.i.d.
4. Solu-Medrol 80 mg IV q8h.
5. Continue the current PO medications.
6. Zithromax 500 mg IV daily.
7. The patient is code level I.
Discussed all of the above with the patient. He seems to understand and agrees with the plan.Will discuss further issues to his abdominal aortic aneurysm and further plans with his positive stress test when the rest of the family is available in the next couple of days.
T1.2:
SERVICE CODE(S): 99221____________________________________________
ICD-10-CM DX CODE(S): RO6.02, J44.1, I50.9___________________________
INCORRECT/MISSING CODE(S):_____________________________________
Correct Answer:

Verified
Correct Answer:
Verified
Q1: AUDIT REPORT T1.1 OFFICE VISIT<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg"
Q2: T1-1A EMERGENCY AND OUTPATIENT RECORD<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg"
Q4: T1-1B CRITICAL CARE SERVICE<br>Dr. Sutton, emergency room
Q5: T1-2A INITIAL HOSPITAL CARE<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg" alt="T1-2A
Q6: T1-2B CONSULTATION<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg" alt="T1-2B CONSULTATION