Exam 4: Processing an Insurance Claim
Exam 1: Health Insurance Specialist Career30 Questions
Exam 2: Introduction to Health Insurance59 Questions
Exam 3: Managed Health Care54 Questions
Exam 4: Processing an Insurance Claim67 Questions
Exam 5: Legal and Regulatory Issues69 Questions
Exam 6: ICD-10-Cm Coding143 Questions
Exam 7: CPT Coding139 Questions
Exam 8: Hcpcs Level II Coding60 Questions
Exam 9: Cms Reimbursement Methodologies75 Questions
Exam 10: Coding for Medical Necessity15 Questions
Exam 11: Essential Cms-1500 Claim Instructions27 Questions
Exam 12: Commercial Insurance18 Questions
Exam 13: Bluecross Blueshield24 Questions
Exam 14: Medicare29 Questions
Exam 15: Medicaid21 Questions
Exam 16: Tricare31 Questions
Exam 17: Workers Compensation20 Questions
Select questions type
When selecting a clearinghouse, providers may also want to determine whether it is accredited by the __________.
Free
(Multiple Choice)
4.8/5  (37)
(37)
Correct Answer:
B
Coordination of benefits (COB) is a provision in __________ health insurance policies intended to keep multiple insurers from paying benefits covered by other policies.
Free
(Multiple Choice)
4.8/5  (35)
(35)
Correct Answer:
C
The computer-to-computer transfer of data between providers and third-party payers (or providers and health care clearinghouses) in a data format agreed upon by sending and receiving parties is called electronic __________.
Free
(Multiple Choice)
4.8/5  (28)
(28)
Correct Answer:
A
When a child lives with both parents, and each parent subscribes to a different health insurance plan, the primary and secondary policies are determined by applying the birthday rule. The individual who holds the primary policy for dependent children is the spouse whose birth __________.
(Multiple Choice)
4.9/5  (30)
(30)
A claims attachment is __________ documentation associated with a health care claim or patient encounter.
(Multiple Choice)
4.9/5  (36)
(36)
Which is the financial record source document used by health care providers and other personnel in a hospital outpatient setting to select codes for treated diagnoses and services rendered to the patient during the current visit?
(Multiple Choice)
4.8/5  (40)
(40)
Which is a computerized permanent record of all financial transactions between the patient and the practice?
(Multiple Choice)
4.8/5  (34)
(34)
Which is an electronic format supported for health care claims transactions?
(Multiple Choice)
4.9/5  (43)
(43)
Which are the amounts owed to a business for services or goods provided?
(Multiple Choice)
5.0/5  (33)
(33)
Which states that third-party debt collectors are prohibited from employing deceptive or abusive conduct in the collection of consumer debts incurred for personal, family, or household purposes?
(Multiple Choice)
4.9/5  (39)
(39)
Which claims are filed according to year and insurance company and include those for which all processing, including appeals, has been completed?
(Multiple Choice)
4.8/5  (39)
(39)
Health insurance plans may include a(n) __________ provision, which means that when the patient has reached that limit for the year, appropriate patient reimbursement to the provider is determined.
(Multiple Choice)
4.9/5  (35)
(35)
Which involves sorting claims upon submission to collect and verify information about the patient and provider?
(Multiple Choice)
4.9/5  (33)
(33)
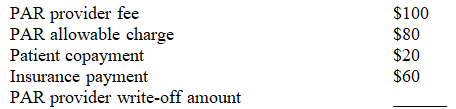
Dr. Smith is a participating provider (PAR) for the ABC Health Insurance Plan. Mary Talley is treated by Dr. Smith in the office, for which a $100 fee is charged. Given the information in the table located below, calculate the PAR provider write-off amount.
(Multiple Choice)
5.0/5  (50)
(50)
Which is the financial record source document used by health care providers and other personnel in a physician's office setting to record treated diagnoses and services rendered to the patient during the current visit?
(Multiple Choice)
4.8/5  (34)
(34)
A remittance advice submitted to the provider electronically is called an electronic remittance advice (ERA), and __________.
(Multiple Choice)
4.8/5  (31)
(31)
When dealing with delinquent claims, it is important to review records to determine whether the claim was paid, was denied, or is pending. A pending claim is considered in __________.
(Multiple Choice)
4.9/5  (35)
(35)
Which is the financial record source document used by health care providers and other personnel to record treated diagnoses and services rendered to the patient during the current visit?
(Multiple Choice)
4.9/5  (36)
(36)
Which claims are organized by year and are generated for providers who do not accept assignment?
(Multiple Choice)
4.8/5  (37)
(37)
Which is considered a financial source document from which an insurance claim is generated?
(Multiple Choice)
4.8/5  (28)
(28)
Showing 1 - 20 of 67
Filters
- Essay(0)
- Multiple Choice(0)
- Short Answer(0)
- True False(0)
- Matching(0)