Exam 4: Processing an Insurance Claim
Exam 1: Health Insurance Specialist Career30 Questions
Exam 2: Introduction to Health Insurance59 Questions
Exam 3: Managed Health Care54 Questions
Exam 4: Processing an Insurance Claim67 Questions
Exam 5: Legal and Regulatory Issues69 Questions
Exam 6: ICD-10-Cm Coding143 Questions
Exam 7: CPT Coding139 Questions
Exam 8: Hcpcs Level II Coding60 Questions
Exam 9: Cms Reimbursement Methodologies75 Questions
Exam 10: Coding for Medical Necessity15 Questions
Exam 11: Essential Cms-1500 Claim Instructions27 Questions
Exam 12: Commercial Insurance18 Questions
Exam 13: Bluecross Blueshield24 Questions
Exam 14: Medicare29 Questions
Exam 15: Medicaid21 Questions
Exam 16: Tricare31 Questions
Exam 17: Workers Compensation20 Questions
Select questions type
Claims adjudication involves making a determination about __________ charges, which is the maximum amount the payer will permit for each procedure or service, according to the patient's policy.
(Multiple Choice)
4.8/5  (37)
(37)
The claim is also checked against the __________, which is an abstract of all recent claims filed on each patient and helps determine whether the patient is receiving concurrent care for the same condition by more than one provider.
(Multiple Choice)
4.9/5  (33)
(33)
When applying the birthday rule, if policyholders have identical birthdays, the policy in effect the __________ is considered primary.
(Multiple Choice)
4.9/5  (39)
(39)
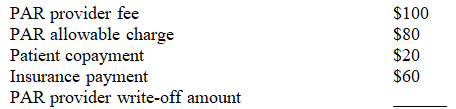
Dr. Jones is a nonparticipating provider (nonPAR) for the ABC Health Insurance Plan. Anne Smith is treated by Dr. Jones in the office, for which a $100 fee is charged. Given the information in the table located below, calculate the nonPAR provider write-off amount.
(Multiple Choice)
4.9/5  (37)
(37)
Which is a legal action that can be used to recover a debt and is usually a last resort for a medical practice?
(Multiple Choice)
4.9/5  (30)
(30)
Which is the fixed amount the patient pays each time he or she receives health care services?
(Multiple Choice)
4.8/5  (37)
(37)
Many physician practices contract out or __________ the delinquent accounts to a full-service collections agency that utilizes collection tactics, including written contacts and multiple calls from professional collectors.
(Multiple Choice)
4.9/5  (38)
(38)
An account receivable that cannot be collected by the provider or a collection agency is called a bad debt. To deduct a bad debt, the amount must have been __________.
(Multiple Choice)
4.8/5  (37)
(37)
Which claims are organized by month and insurance company after submission to the payer, but for which processing is not complete?
(Multiple Choice)
4.9/5  (35)
(35)
Which best assists providers in the overall collection of appropriate reimbursement for services rendered?
(Multiple Choice)
4.8/5  (39)
(39)
Which requires providers to make certain written disclosures concerning all finance charges and related aspects of credit transactions (including disclosing finance charges expressed as an annual percentage rate)?
(Multiple Choice)
4.9/5  (35)
(35)
An appeal is documented as a(n) __________ why a claim should be reconsidered for payment.
(Multiple Choice)
4.8/5  (36)
(36)
Electronic claims are submitted directly to the payer after being checked for accuracy by billing software or a health care clearinghouse, which results in a __________ claim that contains all required data elements needed to process and pay the claim.
(Multiple Choice)
4.9/5  (34)
(34)
Which involves comparing the claim to payer edits and the patient's health plan benefits to verify that the required information is available to process the claim, the claim is not a duplicate, payer rules and procedures have been followed, and procedures performed or services provided are covered benefits?
(Multiple Choice)
4.8/5  (32)
(32)
Procedures and services provided to a patient without proper authorization from the payer, or that were not covered by a current authorization, are called __________ services.
(Multiple Choice)
4.8/5  (38)
(38)
Which establishes the rights, liabilities, and responsibilities of participants in electronic fund transfer systems?
(Multiple Choice)
4.9/5  (31)
(31)
Clearinghouses process claims in an electronic flat file format, which requires conversion of CMS-1500 claims data to a standard format. Providers can also use software to convert claims to an electronic flat file format, also known as a(n) __________, which is a series of fixed-length records (e.g., 25 spaces for patient's name) submitted to payers as a bill for health care services.
(Multiple Choice)
4.7/5  (29)
(29)
A participating provider (PAR) contracts with a health insurance plan and accepts whatever the plan pays for procedures or services performed. This means that PARs __________ allowed to bill patients for the difference between the contracted rate and their normal fee.
(Multiple Choice)
4.8/5  (39)
(39)
Sally Simmons is a patient of Dr. Tyler's. She received preventive services for her annual physical examination on May 17. The third-party payer determined the allowed charge for preventive services to be $100, for which the payer reimbursed the physician 80 percent of that amount. Sally is responsible for paying the remaining 20 percent directly to the physician. Thus, the physician will receive a check in the amount of __________ from the payer, and the patient will pay __________ to the physician.
(Multiple Choice)
4.8/5  (37)
(37)
Showing 21 - 40 of 67
Filters
- Essay(0)
- Multiple Choice(0)
- Short Answer(0)
- True False(0)
- Matching(0)