Exam 16: The Respiratory System: Pulmonary Ventilation
Pressure is the driving force for the movement of air into and out of the lungs. Describe the structure of the thoracic cavity and how that structure is involved in creating the pressures that are important for the movement of air into the lungs.
The thoracic cavity is composed of a number of structures that protect the lungs, including the rib cage, the sternum, the thoracic vertebrae, and a series of muscles. The most important of these muscles are the diaphragm, which separates the thoracic cavity from the abdominal cavity, and the intercostals (internal and external). Other muscles that can be involved in ventilation include the sternocleidomastoids, the scalenes, and the pectoralis minor. The inside of the chest wall and the outside of the lung are lined by an epithelial membrane called the pleura. The visceral (lung)and parietal pleura (chest wall)are in contact with one another, with a small gap between, called the intrapleural space, in which the intrapleural fluid is located. These two membranes are held close to one another as a consequence of surface tension. Thus, the pressure within the intrapleural space (intrapleural pressure)is always negative (because the two membranes are pulling away from one another due especially to the elasticity of the lung). The other important pressures include atmospheric pressure, intra- alveolar pressure, and transpulmonary pressure. It is the difference between atmospheric pressure and intra- alveolar pressure that moves air into and out of the lungs. As lung volume increases, transpulmonary pressure increases (due to the decrease in intrapleural pressure as the chest wall pulls outward from the lung). This increase in transpulmonary pressure will cause the lung to expand and
intra- alveolar pressure to decrease. It is the decrease in intra- alveolar pressure that moves air into the lungs.
An ex- smoker with emphysema has a pulmonary erosion into his intrapleural space. What life- threatening condition is he at imminent risk of developing?
C
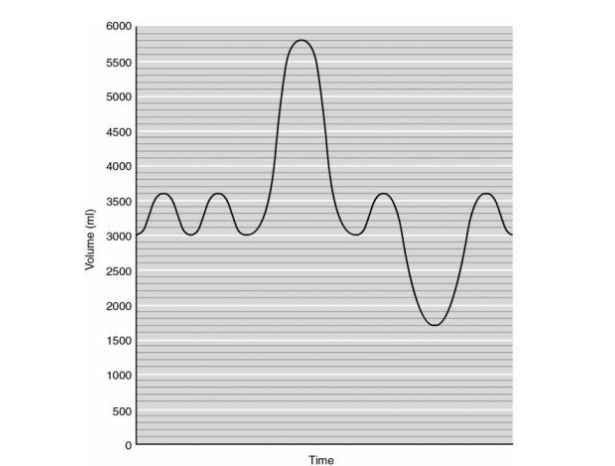 Figure 16.1
-In Figure 16.1, how many mL is the inspiratory capacity?
Figure 16.1
-In Figure 16.1, how many mL is the inspiratory capacity?
A
The transition from the conducting to the respiratory zone in the lungs occurs at the
An increase in sympathetic nervous activity to the smooth muscle cells of the bronchioles will result in a (bronchoconstriction / bronchodilation).
The volume of air in the lungs at rest, between breaths, is called
In an obstructive disease, the lungs can become overinflated because the difficulty in tends to .
Which of the following is responsible for changes in airway resistance that occur in a single breath?
The COPD called emphysema forces the afflicted to exhale through pursed lips to maintain intrabronchial backpressure, thereby preventing
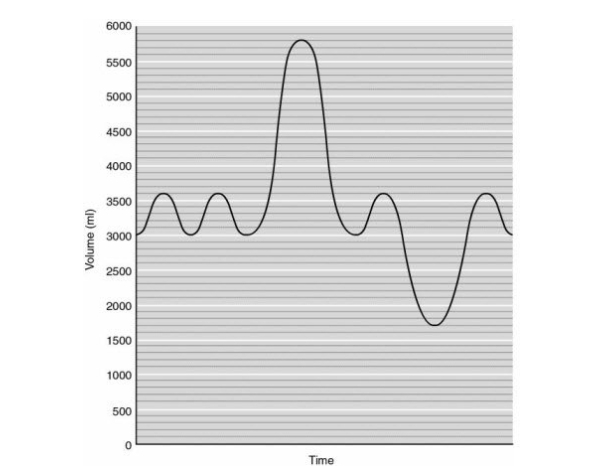 Figure 16.1
-In Figure 16.1, how many mL is the vital capacity?
Figure 16.1
-In Figure 16.1, how many mL is the vital capacity?
A healthy person can normally exhale what percentage of his or her vital capacity in one second?
What is the tidal volume + inspiratory reserve volume + expiratory reserve volume + residual volume called?
A decrease in is indicative of a restrictive pulmonary disease.
Which of the following chemicals will NOT result in a decrease in airway resistance?
What benefit are corticosteroids in the treatment of asthma?
The elasticity of the lungs facilitates expansion during inspiration.
Filters
- Essay(0)
- Multiple Choice(0)
- Short Answer(0)
- True False(0)
- Matching(0)